Cancer in the USA: Understanding America’s Most Critical Health Challenge
Cancer remains one of the most formidable health threats facing Americans today. Every year, millions of people across the United States receive a cancer diagnosis that fundamentally changes their lives. The disease does not discriminate based on age, gender, or economic status.
This devastating illness touches nearly every family in America. Understanding the scope of this challenge is the first step toward protection. The statistics are sobering, yet knowledge empowers us to take meaningful action.
Despite significant advances in medical science, cancer continues to claim hundreds of thousands of American lives annually. However, research shows that many cancer cases are preventable through lifestyle modifications and early detection. This comprehensive guide explores why cancer poses such a significant threat to public health in the United States and what you can do to reduce your personal risk.
Why Cancer Remains a Major Threat to American Public Health
Cancer in the USA represents the second leading cause of death, trailing only heart disease. The American Cancer Society estimates that cancer will claim over 600,000 American lives this year alone. This staggering mortality rate underscores the urgency of understanding and addressing this health crisis.
The disease burden extends far beyond mortality statistics. Cancer affects quality of life for millions of patients and their families. The financial impact devastates households, even those with health insurance coverage.
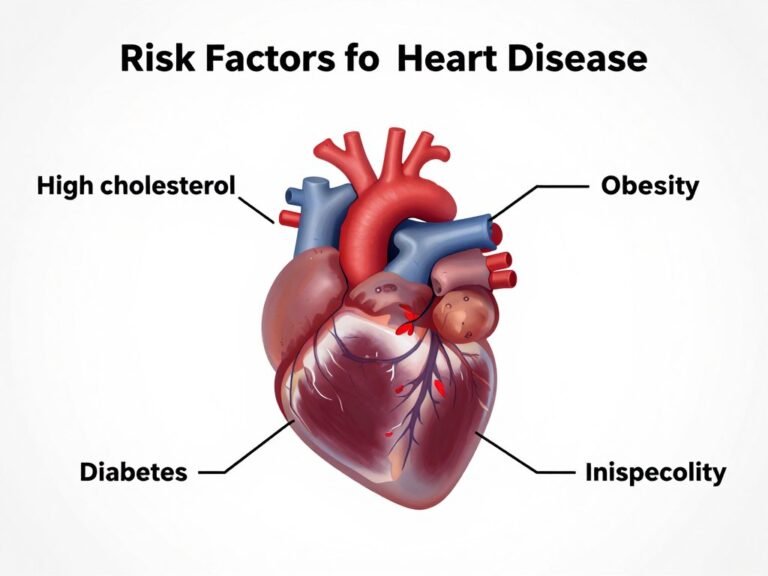
Several factors contribute to cancer’s status as a major health threat in the United States. Our aging population plays a significant role, as cancer risk increases with age. Additionally, lifestyle factors prevalent in American society—including smoking, obesity, poor diet, and physical inactivity—contribute substantially to cancer development.
Key Fact: Approximately 1 in 2 men and 1 in 3 women in the United States will develop some form of cancer during their lifetime. Early detection and prevention strategies can significantly improve survival outcomes.
Environmental exposures and occupational hazards further complicate the cancer landscape. Certain industries expose workers to carcinogenic substances. Air pollution in urban areas contributes to lung cancer risk across populations.
The healthcare system faces challenges in delivering timely screening and treatment. Disparities in access to quality cancer care persist across different socioeconomic and racial groups. These inequities result in worse outcomes for underserved communities.
Cancer’s complexity as a disease category encompasses over 100 different types. Each type requires specialized knowledge, diagnostic approaches, and treatment strategies. This diversity makes prevention and treatment particularly challenging for healthcare providers and researchers.
Why Cancer Poses Unique Challenges
- Multiple disease types with distinct characteristics
- Late-stage diagnosis common for many cancers
- Treatment often requires multi-modal approaches
- Significant financial burden on patients and families
- Long-term survivorship issues and quality of life concerns
- Psychological impact on patients and caregivers
Contributing Risk Factors in American Society
- High rates of tobacco use despite decline trends
- Obesity epidemic affecting two-thirds of adults
- Sedentary lifestyle patterns across age groups
- Processed food consumption and poor dietary habits
- Environmental pollutant exposure in communities
- Insufficient cancer screening participation rates
What Is Cancer: Understanding the Disease at a Cellular Level
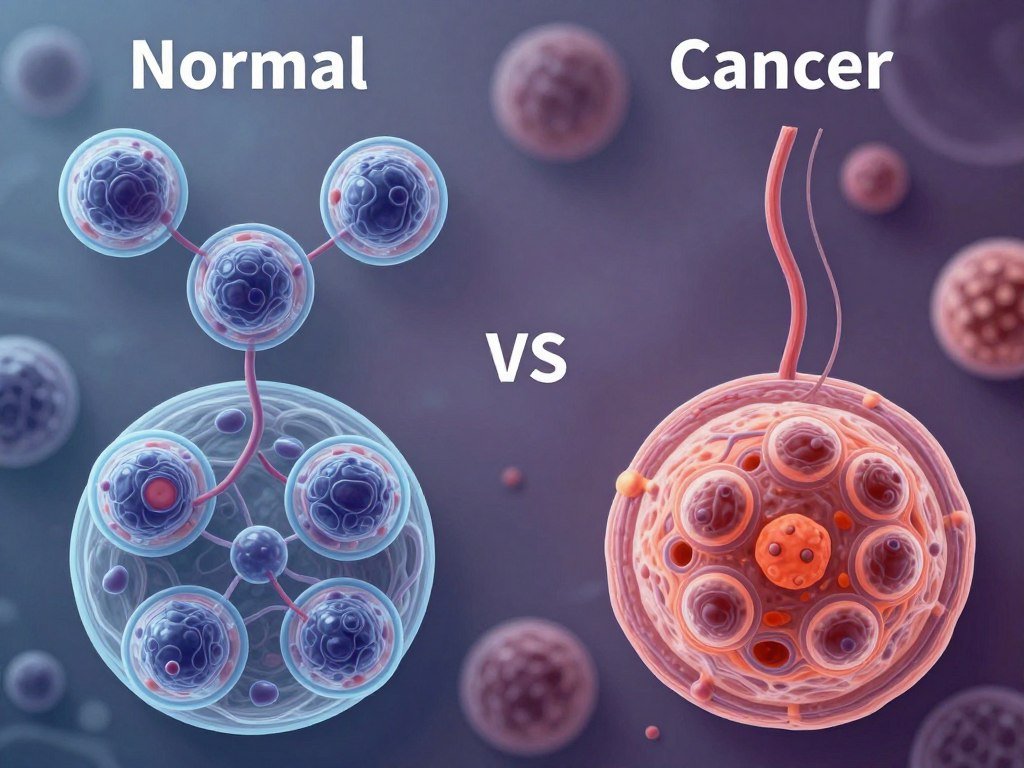
Cancer is not a single disease but rather a collection of related diseases characterized by abnormal cell growth. In a healthy body, cells grow, divide, and die in an orderly fashion. Cancer disrupts this normal process, causing cells to grow and multiply uncontrollably.
When cancer develops, damaged cells survive when they should die. These cells continue dividing without stopping. The accumulation of abnormal cells forms masses of tissue called tumors, though some cancers do not form solid tumors.
Understanding cancer begins with recognizing what happens at the molecular level. Our genetic material, DNA, contains instructions for cell function. When DNA becomes damaged or altered, cells may receive incorrect instructions. These mutations can cause cells to become cancerous.
Medical Definition: Cancer is a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body. Cancer can start almost anywhere in the human body, which contains trillions of cells.
How Normal Cells Transform into Cancer Cells
The transformation from normal cell to cancer cell typically occurs through multiple steps. This process, called carcinogenesis, usually takes many years. Multiple genetic changes must accumulate before a cell becomes fully cancerous.
Normal cells have built-in safeguards that prevent uncontrolled growth. These mechanisms include checkpoints that verify proper cell division and systems that repair damaged DNA. Cancer cells bypass these safety mechanisms through accumulated mutations.
Several characteristics distinguish cancer cells from normal cells. Cancer cells grow in the absence of growth signals that normal cells require. They ignore signals that normally tell cells to stop dividing or die. Cancer cells also invade nearby tissues and spread to distant body parts.
Different Types of Cancer Classifications
Medical professionals classify cancers based on the type of cell where they originate. Carcinomas begin in cells that cover internal and external body surfaces. These represent the most common cancer type, including most breast, lung, and colon cancers.
Sarcomas develop in bone, cartilage, fat, muscle, blood vessels, or other connective tissues. Leukemias start in blood-forming tissue like bone marrow. These cancers cause large numbers of abnormal blood cells to enter the bloodstream.
Lymphomas begin in the immune system’s lymphocytes. These cancers affect lymph nodes and other parts of the immune system. Each cancer type has unique characteristics, risk factors, and treatment approaches.
Benign vs. Malignant Tumors
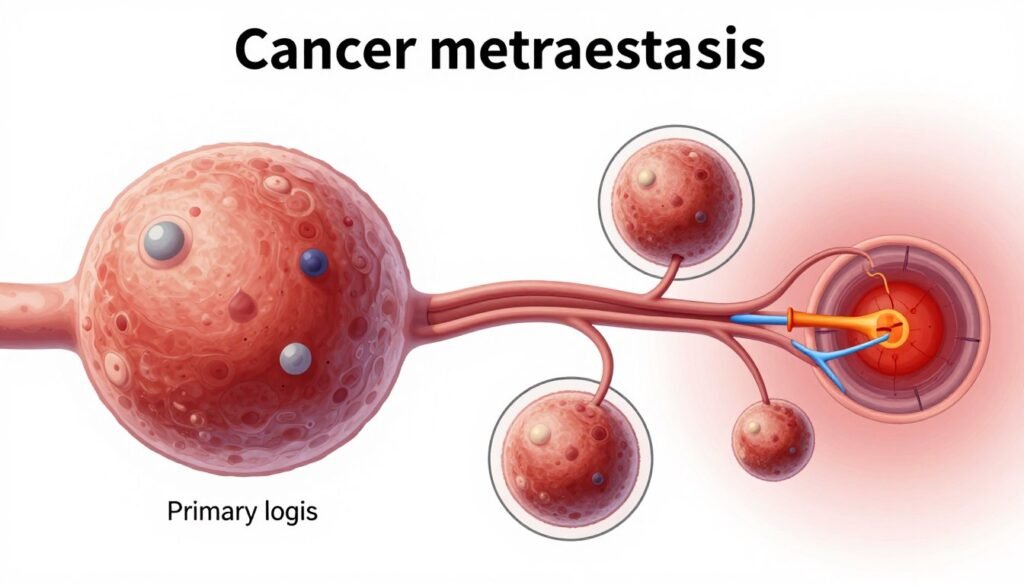
Not all tumors are cancerous. Benign tumors do not spread to other body parts and are not life-threatening in most cases. However, benign tumors can cause problems if they grow large or press on vital organs.
Malignant tumors are cancerous and can invade nearby tissues. These tumors can break away and spread through the bloodstream or lymphatic system. This spreading process, called metastasis, represents one of cancer’s most dangerous characteristics.
What Causes Genetic Mutations
Some people inherit genetic mutations that increase cancer risk. However, most cancer-causing mutations occur during a person’s lifetime. These acquired mutations result from environmental exposures, lifestyle factors, or random errors during cell division.
Tobacco smoke, ultraviolet radiation, and certain chemicals can damage DNA. Chronic inflammation also contributes to genetic damage over time. Some viruses insert their genetic material into human cells, potentially leading to cancer development.
Important Understanding: Cancer development is typically a multi-step process requiring multiple genetic changes. This is why cancer risk increases with age and why prevention strategies focusing on reducing mutation-causing exposures are effective.
Age Groups Most Affected by Cancer in the United States
Cancer incidence rates vary significantly across different age groups in the United States. While cancer can strike at any age, certain patterns emerge when examining cancer cases across the lifespan. Understanding these patterns helps identify populations at greatest risk and informs screening recommendations.
The relationship between age and cancer risk is unmistakable. Cancer incidence rises dramatically with advancing age. More than 80 percent of all cancers in the United States are diagnosed in people aged 55 years and older.
Cancer in Older Adults: The Highest Risk Group
Adults aged 65 years and older bear the greatest cancer burden in America. This age group accounts for approximately 60 percent of new cancer diagnoses annually. The median age at cancer diagnosis is 66 years, reflecting the disease’s strong association with aging.
Several factors explain why cancer risk increases with age. Cells accumulate genetic damage over decades of exposure to cancer-causing agents. The body’s ability to repair damaged DNA declines with age. Additionally, the immune system becomes less effective at identifying and destroying abnormal cells.
Among people aged 65 and older, cancer incidence rates exceed 2,000 cases per 100,000 population. This rate is more than 10 times higher than rates observed in younger adults. The most common cancers in this age group include prostate, breast, lung, and colorectal cancer.

Middle-Aged Adults: A Critical Prevention Window
Adults aged 45 to 64 years represent a critical age group for cancer prevention and early detection. Cancer incidence rates begin rising significantly during these years. Approximately 30 percent of all new cancer cases occur in this age range.
For middle-aged adults, cancer incidence rates range from 400 to 1,000 cases per 100,000 population. The specific rate depends on the precise age within this range. Cancer risk accelerates particularly rapidly after age 50.
This age group faces unique challenges. Many people in their 40s and 50s delay recommended cancer screenings. Work and family obligations may take precedence over preventive health care. However, detecting cancer at this stage often leads to better treatment outcomes than diagnosis in older age.
Breast cancer affects women most commonly during their 50s and 60s. Colorectal cancer incidence rises sharply after age 45, which recently prompted changes to screening guidelines. Lung cancer becomes increasingly common among current and former smokers in this age group.
Screening Recommendations for Middle-Aged Adults: Most cancer screening programs target this age group. Colonoscopy screening now begins at age 45 for average-risk individuals. Mammography recommendations typically start at age 40-50, depending on risk factors. These screenings can detect cancers when they’re most treatable.
Young Adults and Adolescents: Rising Concern
Cancer cases among young adults aged 20 to 39 years remain relatively uncommon but are increasing. This age group accounts for approximately 5 percent of all cancer diagnoses. However, certain cancer types disproportionately affect younger people.
In young adults, cancer incidence rates approximate 60 to 150 cases per 100,000 population. Testicular cancer, thyroid cancer, melanoma, and lymphomas occur more frequently in this demographic. Breast cancer can also affect young women, though less commonly than older women.
Concerning trends show rising cancer rates among younger Americans for certain cancer types. Colorectal cancer incidence has increased among people younger than 50 years. Researchers are working to understand why this shift is occurring.

Children and Adolescents: Rare but Devastating
Childhood cancer remains rare, accounting for less than 1 percent of all cancer diagnoses. Approximately 10,000 children younger than 15 years receive a cancer diagnosis each year in the United States. However, cancer represents the leading disease-related cause of death in children.
Childhood cancers differ significantly from adult cancers. Leukemia is the most common childhood cancer, followed by brain and central nervous system tumors. Many childhood cancers result from genetic mutations that occur early in development rather than accumulated environmental exposures.
Cancer incidence in children is approximately 15 to 20 cases per 100,000 children. While these rates are low compared to adult rates, the impact on affected families is profound. Fortunately, survival rates for childhood cancers have improved dramatically, with more than 80 percent of children now surviving five years or more after diagnosis.
| Age Group | Approximate Incidence Rate (per 100,000) | Percentage of Total Cancer Cases | Most Common Cancer Types |
| Under 20 years | 15-20 | Less than 1% | Leukemia, Brain tumors, Lymphoma |
| 20-39 years | 60-150 | 5% | Breast, Thyroid, Melanoma, Testicular |
| 40-54 years | 400-600 | 15% | Breast, Lung, Colorectal |
| 55-64 years | 900-1,200 | 20% | Lung, Breast, Prostate, Colorectal |
| 65 years and older | 2,000+ | 60% | Prostate, Lung, Breast, Colorectal |
How Cancer Becomes Stressful and Out of Control in the United States

Cancer’s impact extends far beyond physical health challenges. The disease creates cascading stresses that affect patients, families, and the healthcare system. Understanding how cancer becomes overwhelming helps identify support needs and intervention points.
When someone receives a cancer diagnosis, life changes instantly. The word “cancer” triggers profound psychological reactions. Fear, anxiety, and uncertainty dominate the immediate post-diagnosis period. These emotional responses are normal but can become debilitating without proper support.
The Emotional and Psychological Burden
Cancer patients experience unique psychological stresses throughout their illness journey. The diagnosis phase brings shock and disbelief. Many patients describe feeling numb or disconnected from reality. Questions flood their minds about treatment, prognosis, and mortality.
Treatment phases introduce different stressors. Cancer therapies often cause uncomfortable side effects that diminish quality of life. Patients may experience pain, nausea, fatigue, and changes in appearance. These physical challenges compound emotional distress.
Depression and anxiety affect approximately 25 percent of cancer patients at clinically significant levels. Many more experience subclinical symptoms. Fear of cancer recurrence persists even after successful treatment. This ongoing anxiety can last years after completing therapy.
Family members and caregivers also shoulder heavy emotional burdens. They watch loved ones suffer while feeling helpless. Caregiving responsibilities can be physically exhausting and emotionally draining. Many caregivers neglect their own health needs.

Financial Toxicity: The Hidden Crisis
Financial distress represents one of cancer’s most devastating impacts on American families. Medical expenses associated with cancer treatment can be catastrophic. Even patients with health insurance face substantial out-of-pocket costs.
Cancer treatment costs have escalated dramatically in recent decades. Newer targeted therapies and immunotherapies may cost hundreds of thousands of dollars annually. Insurance deductibles, copayments, and coinsurance add up quickly. Many patients exhaust their savings.
Beyond direct medical costs, cancer creates indirect financial burdens. Patients may need to reduce work hours or stop working entirely during treatment. Lost income compounds mounting medical bills. Caregivers may also miss work, further straining family finances.
Studies show that cancer patients file for bankruptcy at rates two and a half times higher than people without cancer. Financial toxicity has become recognized as a serious side effect of cancer treatment. This economic stress negatively impacts treatment adherence and health outcomes.
Financial Reality: The average cost of cancer care in the United States can exceed $150,000 over the course of treatment. Out-of-pocket expenses for insured patients often reach $10,000-$30,000 or more, creating significant financial hardship for most American families.
Healthcare System Challenges and Access Barriers
Navigating the American healthcare system adds another layer of stress for cancer patients. The complexity of insurance coverage creates confusion and frustration. Patients struggle to understand what services are covered and which require prior authorization.
Access to cancer care varies significantly based on geography and insurance status. Rural Americans face particular challenges accessing specialized cancer treatment. Many must travel long distances to reach cancer centers. This travel burden affects treatment compliance and outcomes.
Insurance coverage gaps create treatment delays for many patients. Uninsured and underinsured Americans may postpone necessary care due to cost concerns. Even patients with insurance may face treatment denials or limits on therapy options.
Appointment scheduling challenges frustrate patients and families. Wait times for specialist consultations and diagnostic tests can stretch for weeks. These delays heighten anxiety and may allow cancer to progress. Coordination among multiple providers often falls on patients and families.
System-Level Stressors
- Insurance authorization and coverage disputes
- Long wait times for appointments and procedures
- Poor care coordination among specialists
- Limited access to clinical trials
- Inadequate supportive care services
- Fragmented medical records systems
Personal Impact Factors
- Work disruption and potential job loss
- Relationship strain within families
- Social isolation from friends and community
- Loss of independence and identity
- Difficulty making medical decisions
- Managing complex medication regimens
Treatment Complexity and Side Effect Management
Modern cancer treatment often involves multiple modalities used sequentially or simultaneously. Patients may undergo surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Coordinating these treatments requires expert management and patient vigilance.
Each treatment modality brings potential side effects that require management. Chemotherapy may cause nausea, fatigue, neuropathy, and increased infection risk. Radiation therapy can damage surrounding healthy tissue. Surgery requires recovery time and may result in permanent functional changes.
Managing side effects becomes a full-time job for many patients. They must monitor symptoms, report concerns promptly, and take multiple medications. Nutrition often suffers when appetite decreases or swallowing becomes difficult. These challenges can spiral out of control without proper support.

Disparities That Amplify Stress
Certain populations face additional barriers that make cancer particularly stressful. Racial and ethnic minorities experience disparities in cancer incidence, mortality, and survival. African American men have the highest cancer death rates of any racial or ethnic group in the United States.
These disparities stem from multiple factors. Socioeconomic inequalities affect access to preventive care and screening. Some minority groups have lower rates of health insurance coverage. Cultural and language barriers complicate healthcare navigation.
Environmental justice issues contribute to cancer risk in low-income communities. These neighborhoods may have higher pollution levels and limited access to healthy food options. Residents face occupational hazards at higher rates. These environmental factors compound other stressors.
Geographic disparities also matter. Rural Americans have less access to cancer specialists and treatment facilities. American Indian and Alaska Native populations face particularly severe healthcare access challenges. These disparities mean that cancer becomes even more overwhelming for vulnerable populations.
Addressing the Overwhelm: Research shows that comprehensive psychosocial support, financial counseling, and care navigation services can significantly reduce cancer-related distress. However, these supportive services remain underutilized and underfunded in many healthcare settings.
How to Prevent Cancer: Evidence-Based Protection Strategies

While not all cancers are preventable, research demonstrates that many cancer cases can be avoided through lifestyle modifications and protective measures. The American Cancer Society estimates that approximately 40 percent of cancer cases in the United States are associated with modifiable risk factors.
Prevention represents the most effective approach to reducing cancer burden. Taking action now can significantly decrease your cancer risk over time. The following evidence-based strategies offer powerful protection against multiple cancer types.
Tobacco Avoidance: The Single Most Important Prevention Step
Tobacco use remains the leading preventable cause of cancer death in the United States. Smoking causes approximately 30 percent of all cancer deaths. The carcinogens in tobacco smoke damage DNA and weaken the immune system.
Lung cancer represents the most obvious smoking-related cancer, but tobacco use increases risk for at least 15 different cancer types. These include cancers of the mouth, throat, esophagus, stomach, pancreas, kidney, bladder, and cervix. Even smokeless tobacco products increase cancer risk.
Quitting smoking provides benefits at any age. Within five years of quitting, former smokers cut their lung cancer risk in half compared to current smokers. After 10 years, the risk of dying from lung cancer drops to about half that of continued smokers.
Avoiding secondhand smoke also matters. Nonsmokers exposed to secondhand smoke at home or work increase their lung cancer risk by 20 to 30 percent. Protecting yourself and others from tobacco smoke represents a critical cancer prevention strategy.

Maintaining Healthy Weight and Physical Activity
Obesity has emerged as a major cancer risk factor in the United States. Excess body weight increases risk for at least 13 different cancer types. These include breast cancer in postmenopausal women, colorectal cancer, kidney cancer, esophageal cancer, and pancreatic cancer.
The mechanisms linking obesity to cancer are complex. Excess body fat produces hormones and growth factors that promote cancer development. Fat tissue also creates chronic inflammation, which damages DNA. Obesity affects immune function and other protective mechanisms.
Maintaining a healthy weight throughout life reduces cancer risk significantly. Even modest weight loss provides benefits. Studies show that losing just 5 to 10 percent of body weight can improve health markers and reduce cancer risk factors.
Regular physical activity offers protective effects independent of weight management. Exercise helps regulate hormones, reduces inflammation, and strengthens immune function. The American Cancer Society recommends at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous activity per week.
Physical Activity Benefits: Regular exercise reduces risk of colon cancer by 20-25%, breast cancer by 10-20%, and endometrial cancer by 20-30%. Physical activity also improves outcomes for cancer survivors and reduces recurrence risk.
Adopting a Cancer-Protective Diet
Diet plays a significant role in cancer prevention, though no single food can prevent cancer alone. A dietary pattern rich in plant-based foods provides numerous protective compounds. Vegetables, fruits, whole grains, and legumes contain vitamins, minerals, fiber, and phytochemicals that reduce cancer risk.
Specific dietary recommendations support cancer prevention. Limit consumption of processed meats, which increase colorectal cancer risk. Red meat should be consumed in moderation. The World Health Organization classifies processed meat as carcinogenic to humans.
Excessive alcohol consumption increases risk for several cancer types. Alcohol is linked to cancers of the mouth, throat, esophagus, liver, breast, and colon. The risk increases with the amount consumed. Even moderate drinking raises breast cancer risk in women.
A diet high in ultra-processed foods contributes to obesity and may directly increase cancer risk. These foods often contain additives and chemicals formed during processing. Focusing on whole, minimally processed foods provides optimal cancer protection.
Foods That Protect Against Cancer
- Colorful vegetables and fruits
- Whole grains and fiber-rich foods
- Legumes including beans and lentils
- Nuts and seeds
- Green tea and other antioxidant beverages
- Fatty fish rich in omega-3 fatty acids
- Cruciferous vegetables like broccoli
- Tomatoes rich in lycopene
Foods to Limit or Avoid
- Processed meats and hot dogs
- Excessive red meat consumption
- Sugar-sweetened beverages
- Highly processed snack foods
- Foods high in added sugars
- Deep-fried foods
- Refined grains and white flour products
- Excessive alcohol consumption

Sun Protection and Skin Cancer Prevention
Skin cancer is the most common cancer in the United States, with over 5 million cases treated annually. Most skin cancers result from exposure to ultraviolet radiation from the sun or tanning beds. The good news is that skin cancer is largely preventable.
Sun protection should begin in childhood and continue throughout life. Use broad-spectrum sunscreen with SPF 30 or higher on exposed skin. Apply sunscreen 15 minutes before going outdoors and reapply every two hours. Water-resistant formulas work better during swimming or sweating.
Seek shade during peak sun intensity hours between 10 AM and 4 PM. Wear protective clothing including long-sleeved shirts, pants, and wide-brimmed hats. Sunglasses that block UVA and UVB rays protect the delicate eye area and surrounding skin.
Avoid tanning beds and sun lamps entirely. These devices emit UV radiation that increases skin cancer risk significantly. Studies show that people who use tanning beds before age 35 increase their melanoma risk by 75 percent.
Vaccination Against Cancer-Causing Infections
Several infectious agents cause cancer. Fortunately, vaccines exist that prevent some cancer-causing infections. The HPV vaccine protects against human papillomavirus, which causes cervical, anal, throat, and other cancers. HPV vaccination is recommended for children around age 11 or 12.
The hepatitis B vaccine prevents liver infection that can lead to liver cancer. Hepatitis B vaccination is now routine for infants, but adults at risk should also receive the vaccine. Chronic hepatitis B infection significantly increases liver cancer risk.
These vaccines represent powerful cancer prevention tools. The HPV vaccine could prevent more than 90 percent of HPV-related cancers if vaccination rates were higher. Currently, many eligible adolescents remain unvaccinated, representing a missed prevention opportunity.

Limiting Environmental and Occupational Exposures
Certain environmental exposures increase cancer risk. Radon gas, which seeps into homes from underground, causes lung cancer. Test your home for radon and install mitigation systems if levels are elevated. Radon testing kits are inexpensive and widely available.
Asbestos exposure causes mesothelioma and lung cancer. Many older buildings contain asbestos insulation and materials. If you suspect asbestos in your home, hire certified professionals for testing and removal. Never disturb asbestos materials yourself.
Occupational exposures to carcinogens affect workers in certain industries. Construction workers, farmers, painters, and manufacturing employees may encounter cancer-causing substances. Follow workplace safety protocols and use protective equipment when handling hazardous materials.
Air pollution, particularly fine particulate matter, increases lung cancer risk. While individual control over air quality is limited, you can reduce personal exposure. Avoid exercising near heavy traffic. Use air filters indoors. Support policies that improve air quality.
Cancer Screening: Early Detection Saves Lives
While screening is technically early detection rather than prevention, it prevents cancer deaths by finding disease early when treatment works best. Some screening tests can actually prevent cancer by detecting and removing precancerous conditions.
Colonoscopy screening prevents colorectal cancer by identifying and removing polyps before they become cancerous. Mammography detects breast cancer at early, highly treatable stages. Pap tests and HPV testing prevent cervical cancer through early intervention.
Lung cancer screening with low-dose CT scans benefits current and former heavy smokers aged 50 to 80 years. This screening can detect lung cancer early when surgical cure is possible. Discuss lung cancer screening with your doctor if you have significant smoking history.
Follow screening guidelines appropriate for your age and risk factors. Many Americans skip recommended screenings, missing opportunities for early detection. Regular screening represents one of the most effective ways to reduce cancer mortality.
Take Control of Your Cancer Risk Today
Prevention is the most powerful tool in the fight against cancer. Start implementing these evidence-based strategies now to significantly reduce your risk. Small changes accumulate over time to create substantial protection. Download our comprehensive cancer prevention action plan with specific, achievable goals you can start today.
Is Cancer Treatment Really Helpful? What Doctors Are Saying

This question weighs heavily on the minds of patients facing a cancer diagnosis. The answer depends on many factors, including cancer type, stage at diagnosis, patient health status, and specific treatment approach. Overall, cancer treatment has become increasingly effective over recent decades.
Survival rates for many cancer types have improved dramatically. Five-year survival rates for all cancers combined have increased from approximately 49 percent in the 1970s to nearly 68 percent today. These gains reflect advances in early detection, surgical techniques, radiation therapy, and drug development.
Current State of Cancer Treatment Effectiveness
Treatment effectiveness varies widely among different cancer types. Some cancers respond remarkably well to treatment, with cure rates exceeding 90 percent. These include certain thyroid cancers, prostate cancer detected early, and testicular cancer. Other cancers remain difficult to treat despite medical advances.
Stage at diagnosis profoundly influences treatment outcomes. Cancers detected at localized stages before spreading beyond the primary site have much better prognoses. For example, localized breast cancer has a five-year survival rate above 99 percent. Breast cancer that has spread to distant organs has a five-year survival rate of approximately 29 percent.
These statistics underscore the critical importance of early detection through screening and symptom awareness. Treatment works best when cancer is found early. Delays in diagnosis significantly worsen outcomes for most cancer types.
| Cancer Type | 5-Year Survival Rate (All Stages) | 5-Year Survival Rate (Localized) | Treatment Approach |
| Breast Cancer | 91% | 99% | Surgery, chemotherapy, radiation, hormone therapy |
| Prostate Cancer | 98% | Nearly 100% | Surgery, radiation, hormone therapy, active surveillance |
| Melanoma | 94% | 99% | Surgery, immunotherapy, targeted therapy |
| Colorectal Cancer | 65% | 90% | Surgery, chemotherapy, radiation, targeted therapy |
| Lung Cancer | 22% | 59% | Surgery, chemotherapy, radiation, targeted therapy, immunotherapy |
| Pancreatic Cancer | 11% | 42% | Surgery, chemotherapy, radiation |
What Oncologists Say About Treatment Progress
Leading oncologists express cautious optimism about cancer treatment advances. They emphasize that we have more effective tools than ever before, but challenges remain. Dr. Monica Bertagnolli, Director of the National Cancer Institute, states that precision medicine is transforming cancer care by matching treatments to specific tumor characteristics.
Immunotherapy represents one of the most exciting recent advances. These treatments harness the body’s immune system to fight cancer. For certain cancers, immunotherapy has produced remarkable results where other treatments failed. Some patients with advanced melanoma or lung cancer have achieved long-term survival thanks to immunotherapy.
Targeted therapy has revolutionized treatment for cancers driven by specific genetic mutations. Drugs designed to block particular molecular pathways can be highly effective with fewer side effects than traditional chemotherapy. These precision approaches work best when tumor genetic testing identifies actionable mutations.
Oncologists acknowledge that not all patients benefit equally from new therapies. Some cancers remain resistant to current treatments. Research continues to identify new therapeutic targets and develop novel treatment approaches. Clinical trials offer access to promising experimental therapies.
“We’ve made tremendous progress in cancer treatment over the past few decades. For many patients, cancer has become a manageable chronic disease rather than an automatic death sentence. However, we still have much work to do, particularly for aggressive cancers that don’t respond well to current therapies.”
The Role of Combination Therapy
Modern cancer treatment often combines multiple approaches to maximize effectiveness. Surgery removes the primary tumor. Radiation therapy targets cancer cells in specific body areas. Chemotherapy reaches cancer cells throughout the body. This multi-pronged approach improves outcomes for many patients.
Combination therapy requires careful coordination among specialists. Medical oncologists, surgical oncologists, and radiation oncologists work together to develop comprehensive treatment plans. This multidisciplinary approach has become the standard of care at cancer centers.
The sequence and timing of different treatment modalities matter. Neoadjuvant therapy given before surgery can shrink tumors, making them easier to remove. Adjuvant therapy administered after surgery destroys remaining cancer cells. Oncologists carefully plan treatment sequences based on evidence and individual patient factors.

Personalized Medicine and Genetic Testing
Genetic testing has transformed cancer treatment decision-making. Tumor genetic profiling identifies specific mutations driving cancer growth. This information guides treatment selection, allowing oncologists to choose therapies most likely to work for each patient’s unique cancer.
Some genetic mutations predict excellent response to specific drugs. Breast cancers with HER2 overexpression respond to HER2-targeted therapies. Lung cancers with EGFR mutations benefit from EGFR inhibitors. Matching treatment to tumor genetics improves outcomes while avoiding ineffective therapies.
Liquid biopsies represent an emerging technology that detects cancer DNA in blood samples. These tests can monitor treatment response and detect recurrence earlier than imaging scans. As liquid biopsy technology advances, it may enable more personalized treatment adjustments.
Quality of Life Considerations
Treatment effectiveness encompasses more than survival statistics. Quality of life during and after treatment matters greatly to patients. Oncologists increasingly emphasize preserving function and minimizing treatment toxicity while maintaining effectiveness.
Supportive care has improved dramatically. Better anti-nausea medications make chemotherapy more tolerable. Pain management techniques help patients maintain comfort. Rehabilitation services address physical limitations. Psychological support addresses emotional and mental health needs.
For some patients, particularly those with advanced disease, quality of life takes precedence over aggressive treatment. Palliative care focuses on symptom management and comfort. This approach does not mean giving up—it means prioritizing what matters most to the patient.
Survivorship care addresses the needs of people who have completed cancer treatment. Many survivors experience long-term effects from treatment. Comprehensive survivorship programs help manage these issues and monitor for recurrence. The growing population of cancer survivors demonstrates treatment success.
Treatment Decision Factors: Oncologists consider multiple factors when recommending treatment including cancer type and stage, patient age and overall health, potential side effects, patient preferences and values, and available clinical trial options. Shared decision-making between doctors and patients leads to better outcomes and satisfaction.
Challenges and Limitations
Despite progress, significant challenges remain in cancer treatment. Some cancers, particularly pancreatic cancer and certain brain tumors, remain difficult to treat effectively. Metastatic disease continues to be challenging, though new therapies have improved outcomes for some advanced cancers.
Treatment resistance frustrates both patients and doctors. Cancer cells can adapt and become resistant to therapies that initially worked. Researchers work to understand resistance mechanisms and develop strategies to overcome them.
Access to cutting-edge treatments remains unequal. The newest therapies are often extremely expensive and may not be covered by insurance. Clinical trial availability varies by location. These disparities mean that treatment effectiveness in real-world settings may differ from ideal scenarios.
Side effects from treatment, while often manageable, can be severe. Chemotherapy causes fatigue, nausea, and increased infection risk. Radiation may damage healthy tissue near the treatment area. Immunotherapy can cause immune system overreaction. Weighing benefits against risks requires careful consideration.
Treatment Success Factors
- Early stage at diagnosis
- Cancer type with good treatment response
- Access to specialized cancer center
- Comprehensive multidisciplinary care
- Patient overall health and fitness
- Treatment compliance and adherence
- Genetic profile matching targeted therapies
- Strong support system
Ongoing Treatment Challenges
- Treatment resistance development
- Metastatic disease management
- Managing severe side effects
- High cost of new therapies
- Limited treatment options for some cancers
- Recurrence after initial treatment success
- Access disparities for underserved populations
- Balancing quality of life with survival
The Bottom Line on Treatment Effectiveness
Cancer treatment is undeniably helpful for most patients. Advances in surgery, radiation, chemotherapy, targeted therapy, and immunotherapy have dramatically improved outcomes. Many people survive cancer and return to normal life. Even those with advanced disease often gain valuable time with good quality of life.
However, treatment effectiveness varies significantly based on individual circumstances. Not every patient experiences the same outcomes. Cancer remains a serious disease that requires aggressive treatment, and that treatment can be difficult to endure.
The medical community continues working to improve treatment effectiveness while reducing side effects. Clinical trials test promising new approaches. Research into cancer biology reveals new therapeutic targets. The future of cancer treatment looks increasingly hopeful.
For anyone facing a cancer diagnosis, partnering with experienced oncologists and seeking care at comprehensive cancer centers offers the best chance for successful treatment. Ask questions, explore all options including clinical trials, and make decisions aligned with your values and goals.
Cancer Statistics Over 100 Years: A Century of Data
Examining cancer statistics over the past century reveals dramatic changes in cancer incidence, mortality, and survival. These trends reflect evolving risk factors, diagnostic capabilities, and treatment advances. Understanding this historical context helps us appreciate progress while recognizing ongoing challenges.
In the early 20th century, cancer was less common than infectious diseases. Shorter life expectancy meant fewer people lived long enough to develop cancer. As public health improved and life expectancy increased, cancer became more prevalent. Today, cancer ranks as a leading cause of death because people live longer.
The following table presents cancer statistics spanning approximately 100 years in the United States. Data from earlier decades are estimates based on available records, as comprehensive cancer registries were not established until later in the 20th century. Modern data comes from authoritative sources including the National Cancer Institute and American Cancer Society.
| Decade | Estimated New Cases (Annual) | Estimated Deaths (Annual) | Death Rate per 100,000 | 5-Year Survival Rate | Most Common Cancers |
| 1920s | ~200,000 | ~125,000 | ~110 | ~20% | Stomach, Lung, Breast |
| 1930s | ~275,000 | ~150,000 | ~120 | ~25% | Stomach, Lung, Breast |
| 1940s | ~350,000 | ~175,000 | ~130 | ~30% | Lung, Breast, Colorectal |
| 1950s | ~500,000 | ~250,000 | ~150 | ~35% | Lung, Breast, Colorectal |
| 1960s | ~650,000 | ~290,000 | ~155 | ~39% | Lung, Breast, Colorectal |
| 1970s | ~800,000 | ~365,000 | ~170 | ~49% | Lung, Breast, Colorectal |
| 1980s | ~1,000,000 | ~460,000 | ~190 | ~53% | Lung, Breast, Colorectal |
| 1990s | ~1,250,000 | ~530,000 | ~200 | ~60% | Breast, Lung, Prostate |
| 2000s | ~1,450,000 | ~560,000 | ~190 | ~65% | Breast, Lung, Prostate |
| 2010s | ~1,700,000 | ~600,000 | ~160 | ~67% | Breast, Lung, Prostate |
| 2020s | ~1,900,000 | ~610,000 | ~145 | ~68% | Breast, Lung, Prostate |
Key Historical Trends and Insights
Several important patterns emerge from this century of cancer data. The absolute number of cancer cases has increased substantially, primarily due to population growth and aging. The United States population has more than tripled since the 1920s, and the median age has increased significantly.
However, age-adjusted death rates per 100,000 population tell a more encouraging story. Death rates peaked in the early 1990s and have declined approximately 30 percent since then. This decline represents prevention efforts, earlier detection, and improved treatment saving millions of lives.
Survival rates have improved dramatically. The five-year survival rate for all cancers combined has increased from about 20 percent in the 1920s to nearly 70 percent today. This improvement reflects advances across prevention, screening, surgery, radiation, and systemic therapy.
Historic Milestone: Since the peak in 1991, cancer death rates have fallen by approximately 33 percent, translating to an estimated 3.8 million cancer deaths averted through 2021. This represents one of the great public health achievements of modern medicine.
Shifting Cancer Patterns Over Time
The types of cancer affecting Americans have shifted over the century. Stomach cancer was once among the most common cancers but has declined dramatically. This decrease relates to improved food preservation, reduced salt consumption, and treatment of H. pylori bacteria.
Lung cancer emerged as a major killer beginning in the mid-20th century, paralleling the rise of cigarette smoking. Lung cancer incidence peaked in the 1980s for men and the 2000s for women. Rates are now declining as smoking prevalence decreases, though lung cancer remains the leading cause of cancer death.
Prostate cancer diagnosis increased dramatically after PSA testing became common in the early 1990s. Many of these detected cancers are slow-growing and might never have caused symptoms. This overdiagnosis phenomenon has led to more conservative screening approaches.
Colorectal cancer incidence and mortality have declined substantially since the 1980s, primarily due to screening colonoscopy. Removing precancerous polyps prevents cancer development. However, concerning increases in colorectal cancer among younger adults represent a new challenge.
Major Advances Contributing to Progress
- Decline in smoking rates since 1960s
- Widespread mammography screening
- Colonoscopy and polyp removal
- HPV and hepatitis B vaccination
- Improved surgical techniques
- Targeted chemotherapy regimens
- Radiation therapy precision
- Immunotherapy development
- Targeted molecular therapies
Emerging Challenges
- Obesity epidemic impact
- Rising cancer rates in young adults
- Health disparities among minorities
- Access to expensive new therapies
- Environmental carcinogen exposure
- Aging population increasing cancer burden
- Healthcare system capacity constraints
- Treatment resistance development
- Long-term survivorship needs
Demographic Differences in Progress
Progress has not been equal across all population groups. African Americans have experienced higher cancer death rates than whites throughout most of the past century. While death rates have declined for both groups, disparities persist. African American men have the highest cancer mortality rate of any racial or ethnic group.
Socioeconomic factors significantly influence cancer outcomes. People living in poverty have higher cancer mortality rates. Limited access to screening and treatment, along with higher prevalence of risk factors, contribute to these disparities. Addressing these inequities remains a public health priority.
Geographic disparities have also persisted. Rural Americans have less access to cancer care and experience worse outcomes for many cancer types. Distance to specialized cancer centers creates barriers to optimal treatment. Telemedicine and mobile screening units offer potential solutions.
Looking Forward: Future Projections
Cancer cases are projected to continue increasing in absolute numbers as the population ages. The number of cancer survivors is also growing, creating new healthcare needs. An estimated 18 million Americans alive today have a history of cancer.
However, continued progress in prevention and treatment could further reduce death rates. If current trends continue, cancer mortality rates may decline another 20 to 30 percent over the next few decades. Achieving this goal requires sustained investment in research, equitable access to care, and effective prevention strategies.
Precision medicine holds promise for further improving outcomes. As we better understand cancer biology and genetics, treatments will become increasingly personalized and effective. Artificial intelligence may enhance early detection and treatment selection. These advances could accelerate the pace of progress.
Is Cancer Curable or Chronic? Understanding Disease Trajectories

The question of whether cancer is curable or chronic does not have a single answer. Cancer encompasses over 100 different diseases with vastly different characteristics. Some cancers are highly curable, while others behave more like chronic conditions requiring ongoing management.
Understanding these distinctions helps set realistic expectations and informs treatment decisions. The concepts of cure, remission, and chronic disease management all apply to cancer in different contexts. Modern medicine has transformed some previously fatal cancers into manageable chronic conditions.
What Does Cancer Cure Mean?
In medical terms, cancer cure typically means the disease has been completely eliminated from the body with no evidence of remaining cancer cells. Doctors often use the term “no evidence of disease” (NED) to describe this status. However, proving absolute cure is challenging because microscopic cancer cells may persist undetected.
Oncologists generally consider patients cured if they remain cancer-free for a specific period after treatment, typically five to ten years. The five-year survival milestone is commonly used because most recurrences happen within five years. However, some cancers can recur after longer periods.
Cure rates vary tremendously by cancer type and stage. Certain cancers detected early have cure rates exceeding 90 percent. These include thyroid cancer, melanoma in situ, and prostate cancer confined to the prostate. Early-stage breast and colorectal cancers also have high cure rates when treated appropriately.
Cure Definition: Medical professionals typically define cancer cure as remaining free of disease for five years after treatment completion with no signs of recurrence. However, some cancer types require longer surveillance periods, and “cure” remains a statistical probability rather than absolute certainty.
Highly Curable Cancers
Several cancer types are considered highly curable, especially when detected early. Testicular cancer has a cure rate above 95 percent, even for many advanced cases. This represents one of medicine’s great success stories. Aggressive chemotherapy regimens developed in the 1970s transformed testicular cancer from often fatal to highly curable.
Thyroid cancer, particularly papillary thyroid cancer, has an excellent prognosis. More than 98 percent of patients with localized thyroid cancer survive five years or more. Treatment typically involves surgery to remove the thyroid, sometimes followed by radioactive iodine therapy.
Early-stage skin cancers are nearly always curable. Basal cell carcinoma and squamous cell carcinoma rarely spread and can be surgically removed with high cure rates. Even melanoma, a more dangerous skin cancer, has a five-year survival rate above 99 percent when caught early before spreading.
Hodgkin lymphoma represents another cancer type with high cure rates. Modern combination chemotherapy and radiation therapy cure approximately 85 to 90 percent of patients. This success demonstrates the power of evidence-based cancer treatment protocols.

Cancer as a Chronic Disease
For some patients, cancer becomes a chronic condition managed over many years rather than cured. This concept has gained recognition as treatment advances allow people to live longer with cancer. Some cancers that were once rapidly fatal can now be controlled for extended periods.
Chronic myeloid leukemia (CML) exemplifies cancer’s transformation into a chronic disease. Targeted therapy with tyrosine kinase inhibitors has revolutionized CML treatment. Patients who once faced poor prognoses now often live normal lifespans with daily medication. The cancer persists but remains controlled.
Some slow-growing prostate cancers are managed with active surveillance rather than immediate treatment. Low-risk prostate cancer may never progress to cause problems. Monitoring the cancer closely while avoiding treatment side effects represents a chronic disease management approach.
Metastatic breast cancer has become increasingly manageable as a chronic condition for many patients. While not curable once it spreads, sequential treatment regimens can control disease progression for years. Some patients live decades with metastatic breast cancer through ongoing therapy.
Characteristics of Curable Cancers
- Detected at early, localized stages
- Complete surgical removal possible
- Highly responsive to chemotherapy or radiation
- Specific genetic features allowing targeted therapy
- Slow-growing tumors caught before spread
- Low-grade cancers with minimal aggressiveness
- Effective multi-modality treatment protocols
- No distant metastases at diagnosis
Characteristics of Chronic Cancers
- Metastatic disease present at diagnosis
- Slow-growing with long natural history
- Controllable but not eliminable with current therapy
- Require ongoing maintenance treatment
- Respond to sequential therapy lines
- Compatible with good quality of life during treatment
- Balanced approach between control and side effects
- Long-term disease stability achievable
The Role of Remission
Remission represents an important concept in cancer care. Complete remission means all signs and symptoms of cancer have disappeared. Tests show no evidence of disease. However, remission differs from cure because cancer may still return.
Partial remission means cancer has decreased in size or extent but has not completely disappeared. Patients in partial remission may experience symptom relief and improved quality of life even though cancer persists. This situation reflects cancer as a chronic, managed condition.
Remission duration varies widely. Some patients remain in remission for decades without recurrence. Others experience relatively short remissions before cancer returns. Long-term remission approaching ten years or more is often functionally equivalent to cure, though doctors avoid using that term definitively.
Understanding Remission: Complete remission means no detectable cancer remains, but does not guarantee cure since microscopic disease may persist. Doctors use remission terminology because cancer can potentially return, though many patients in long-term remission never experience recurrence.
Cancer Recurrence Patterns
Cancer recurrence happens when cancer returns after treatment and remission. Recurrence can occur locally at the original tumor site, regionally in nearby lymph nodes or tissues, or distantly as metastatic disease in other organs. The pattern and timing of recurrence provide information about prognosis and treatment options.
Local and regional recurrences may still be curable with additional treatment. Distant metastatic recurrence typically represents incurable disease, though long-term control may be achievable. Understanding recurrence risk helps patients and doctors plan appropriate surveillance schedules.
Risk of recurrence varies by cancer type, stage, and treatment received. High-grade cancers have greater recurrence risk than low-grade cancers. Cancers with lymph node involvement at diagnosis carry higher recurrence risk. Recurrence risk generally decreases with time, though never reaches zero.

The Psychological Impact of Cure Versus Chronic
The distinction between cure and chronic disease significantly affects patients psychologically. Hope for cure motivates patients through difficult treatment. Achieving cure provides closure and allows survivors to move forward. However, fear of recurrence often persists even after cure is likely.
Living with cancer as a chronic disease requires different psychological adjustment. Patients must accept ongoing treatment and surveillance while maintaining quality of life. This adjustment can be challenging but allows many people to live well for extended periods.
Some patients struggle with ambiguity inherent in cancer care. The inability to definitively declare cure creates uncertainty. Support from mental health professionals helps patients cope with this ongoing stress. Cancer support groups connect people facing similar challenges.
Factors Influencing Cure Potential
Multiple factors determine whether a specific cancer is curable. Cancer type represents the most fundamental factor. Some cancer types are inherently more aggressive and difficult to cure. Biology matters more than any other single factor.
Stage at diagnosis profoundly impacts cure potential. Localized cancers before metastasis offer the best cure opportunities. Once cancer spreads to distant organs, cure becomes unlikely with current treatments, though exceptions exist.
Tumor grade and genetic characteristics influence curability. Low-grade tumors with favorable genetics respond better to treatment. High-grade tumors with aggressive features are harder to cure. Molecular testing increasingly informs prognosis and treatment selection.
Patient factors also matter. Younger patients generally tolerate aggressive treatment better. Better overall health status improves ability to withstand curative therapy. However, age alone should not determine treatment approach—biological age matters more than chronological age.
| Cancer Type | Curability Status | 5-Year Survival (Localized) | Management Approach |
| Testicular Cancer | Highly Curable | 99% | Curative intent treatment |
| Thyroid Cancer | Highly Curable | Nearly 100% | Curative intent treatment |
| Melanoma (Early) | Highly Curable | 99% | Curative intent treatment |
| Breast Cancer (Early) | Often Curable | 99% | Curative intent treatment |
| Prostate Cancer (Low Risk) | Often Curable or Chronic | Nearly 100% | Curative or surveillance |
| Chronic Myeloid Leukemia | Chronic Disease | 90% | Long-term disease control |
| Metastatic Breast Cancer | Chronic Disease | 29% (Distant) | Ongoing management |
| Pancreatic Cancer | Rarely Curable | 42% | Aggressive treatment, often palliative |
The Future of Cancer as a Chronic Disease
Medical advances continue transforming more cancers into chronic, manageable conditions. Targeted therapies and immunotherapies offer long-term disease control for some previously untreatable cancers. As new treatments emerge, the concept of cancer as chronic disease will likely expand.
This shift requires changes in healthcare delivery. Chronic cancer management demands different support structures than acute curative treatment. Long-term medication adherence, side effect management, and quality of life optimization become priorities. Healthcare systems are adapting to meet these evolving needs.
For patients and families, understanding whether cancer is curable or chronic helps frame expectations and goals. Curative treatment aims for complete disease elimination. Chronic disease management focuses on maximizing life quality and duration. Both approaches are valuable and appropriate in different circumstances.
Understand Your Cancer Prognosis
Every cancer diagnosis is unique. Discuss your specific prognosis, treatment goals, and realistic outcomes with your oncology team. Understanding whether your cancer is potentially curable or more appropriately managed as a chronic condition helps align treatment decisions with your personal values and goals. Seek second opinions when facing major treatment decisions.
Lifestyle and Food Choices That Increase Cancer Risk
Many cancers develop due to lifestyle choices and environmental exposures accumulated over decades. Research has identified specific behaviors and dietary patterns that significantly increase cancer risk. Understanding these risk factors empowers people to make informed choices that protect their health.
The encouraging reality is that many cancer risk factors are modifiable. While we cannot change our genetics or completely avoid all environmental hazards, we have substantial control over lifestyle and dietary choices. These decisions compound over time to either increase or decrease cancer risk.
Tobacco Use: The Leading Preventable Cancer Cause
Tobacco use stands as the single most significant preventable cause of cancer. Smoking causes approximately 30 percent of all cancer deaths and 80 percent of lung cancer deaths in the United States. The carcinogens in tobacco smoke damage DNA throughout the body, not just in the lungs.
Cigarette smoking increases risk for at least 15 different cancer types. Beyond lung cancer, smoking causes cancers of the mouth, throat, voice box, esophagus, stomach, pancreas, kidney, bladder, cervix, and certain types of leukemia. The risk increases with duration and intensity of smoking.
Smokeless tobacco products including chewing tobacco and snuff also cause cancer. These products increase risk of cancers of the mouth, esophagus, and pancreas. There is no safe tobacco product. All forms of tobacco use increase cancer risk.
Secondhand smoke exposure harms nonsmokers. People regularly exposed to secondhand smoke have increased lung cancer risk. Children exposed to secondhand smoke face higher cancer risks later in life. Protecting others from tobacco smoke represents an important public health priority.

Alcohol Consumption and Cancer Risk
Alcohol consumption increases risk for several cancer types. The more alcohol consumed, the higher the risk. Even moderate drinking elevates risk for certain cancers, particularly breast cancer in women. No level of alcohol consumption is completely safe from a cancer risk perspective.
Alcohol is causally linked to cancers of the mouth, throat, voice box, esophagus, liver, breast, and colon. The mechanisms are complex. Alcohol is metabolized to acetaldehyde, a toxic compound that damages DNA. Alcohol also increases estrogen levels and impairs nutrient absorption.
Combined tobacco and alcohol use multiplies cancer risk beyond the additive effect of either substance alone. People who both smoke and drink heavily have dramatically elevated risk of head and neck cancers. Avoiding both substances provides the greatest protection.
Recommendations suggest limiting alcohol consumption. If you choose to drink, limit intake to no more than one drink per day for women or two drinks per day for men. Many cancer prevention experts recommend avoiding alcohol entirely given the cancer risk.
Alcohol and Breast Cancer: Women who consume two to three alcoholic drinks per day have approximately 20 percent higher breast cancer risk compared to women who don’t drink. Risk increases progressively with consumption. Even light drinking (up to one drink per day) modestly elevates risk.
Obesity and Excess Body Weight
Obesity has emerged as one of the most significant cancer risk factors in the United States. Excess body weight increases risk for at least 13 different cancer types. These include postmenopausal breast cancer, colorectal cancer, endometrial cancer, esophageal cancer, kidney cancer, liver cancer, pancreatic cancer, and others.
The mechanisms linking obesity to cancer are multifaceted. Adipose tissue produces excess estrogen, which promotes certain cancers. Obesity creates chronic low-grade inflammation that damages DNA. Insulin resistance and elevated growth factors promote cell proliferation. Obesity also affects immune system function.
Body mass index (BMI) over 30 defines obesity. However, body fat distribution matters too. Central obesity with excess abdominal fat appears particularly risky. Waist circumference provides a simple measure of central obesity. Men with waist circumference over 40 inches and women over 35 inches face elevated health risks.
Weight gain during adulthood increases cancer risk even without reaching obesity thresholds. Maintaining stable weight throughout adult years provides protection. Even modest weight loss reduces risk in people who are overweight or obese. Studies show that losing 5 to 10 percent of body weight improves health markers.
Physical Inactivity and Sedentary Behavior
Physical inactivity represents an independent cancer risk factor beyond its contribution to obesity. Sedentary lifestyle increases risk for colon cancer, breast cancer, and endometrial cancer. The protective effects of physical activity operate through multiple mechanisms including hormone regulation and immune enhancement.
Americans spend increasing amounts of time sitting. Extended periods of sitting, even among people who exercise regularly, may increase cancer risk. Breaking up prolonged sitting with brief activity breaks appears beneficial. Standing desks and walking meetings offer simple strategies to reduce sitting time.
The modern environment discourages physical activity. Car dependence, desk jobs, and screen-based entertainment promote sedentary behavior. Counteracting these environmental pressures requires conscious effort. Building physical activity into daily routines makes consistency easier.
Dietary Patterns That Increase Cancer Risk
Certain dietary patterns elevate cancer risk. The typical American diet high in processed foods, red meat, sugar, and unhealthy fats increases cancer risk. This dietary pattern also promotes obesity, compounding cancer risk through multiple pathways.
Processed meat consumption increases colorectal cancer risk. Processed meats include bacon, sausage, hot dogs, deli meats, and other preserved meat products. The World Health Organization classifies processed meat as carcinogenic to humans. Even modest consumption increases risk, and higher consumption further elevates risk.
High red meat consumption also increases cancer risk, particularly for colorectal cancer. Red meat includes beef, pork, and lamb. Grilling or barbecuing meat at high temperatures creates carcinogenic compounds. Limit red meat consumption and choose healthier protein sources more often.
Diets high in added sugars and refined carbohydrates promote weight gain and obesity. Sugar-sweetened beverages contribute empty calories without nutritional value. High sugar consumption increases risk for several cancers through obesity promotion and metabolic effects.
High-Risk Dietary Choices
- Regular processed meat consumption
- Excessive red meat intake
- Sugar-sweetened beverages
- Ultra-processed snack foods
- Deep-fried foods
- Excessive alcohol consumption
- Diets low in vegetables and fruits
- High-calorie, low-nutrient foods
- Excessive salt intake
- Charred or heavily grilled meats
High-Risk Lifestyle Factors
- Any tobacco use
- Excessive sun exposure without protection
- Physical inactivity and sedentary behavior
- Insufficient sleep duration and quality
- Chronic high stress levels
- Exposure to environmental pollutants
- Occupational carcinogen exposure
- Unprotected exposure to infectious agents
- Inadequate cancer screening participation
- Ignoring persistent symptoms
Ultra-Processed Foods and Cancer
Ultra-processed foods dominate the modern American diet. These products contain ingredients not typically used in home cooking, including artificial flavors, colors, emulsifiers, and preservatives. Research increasingly links ultra-processed food consumption to cancer risk.
Several mechanisms may explain this association. Ultra-processed foods often contain potentially carcinogenic additives. Processing creates harmful compounds. These foods are typically calorie-dense and nutrient-poor, promoting obesity. They may also disrupt metabolic health and alter gut microbiota.
Common ultra-processed foods include packaged snacks, sodas, instant noodles, most breakfast cereals, reconstituted meat products, and many ready-to-eat meals. Reading ingredient lists helps identify ultra-processed products. Long lists of unfamiliar ingredients indicate high processing levels.
Replacing ultra-processed foods with whole, minimally processed foods reduces cancer risk. Choose fresh vegetables, fruits, whole grains, legumes, nuts, and minimally processed meats and dairy. Cooking at home using basic ingredients minimizes exposure to processed food additives and chemicals.
Environmental and Occupational Exposures
While less modifiable than diet and lifestyle, certain environmental exposures increase cancer risk. Air pollution, particularly fine particulate matter, increases lung cancer risk. People living in areas with high pollution levels face elevated risk. Supporting clean air policies benefits entire communities.
Radon exposure in homes causes lung cancer, particularly among smokers. Radon is a colorless, odorless gas that seeps into buildings from underground. Testing homes for radon and installing mitigation systems when needed protects families. Radon test kits are inexpensive and readily available.
Occupational exposures affect workers in certain industries. Asbestos, benzene, formaldehyde, and numerous other workplace chemicals increase cancer risk. Following workplace safety protocols, using protective equipment, and supporting strong occupational health regulations protect workers.
Pesticide exposure may increase cancer risk, though evidence varies by specific chemicals. Washing produce removes surface residues. Choosing organic produce for foods with high pesticide residues (the “dirty dozen”) reduces exposure. However, eating conventional produce is better than not eating vegetables and fruits at all.
Important Perspective: While environmental exposures contribute to cancer risk, lifestyle factors including tobacco use, obesity, alcohol consumption, and diet represent more significant controllable risks for most people. Focus first on major lifestyle modifications for maximum cancer risk reduction.
Sleep Deprivation and Chronic Stress
Emerging research suggests that chronic sleep deprivation may increase cancer risk. Sleep disruption affects hormone regulation, immune function, and DNA repair mechanisms. Night shift work that disrupts circadian rhythms has been classified as a probable carcinogen by the World Health Organization.
Most adults need seven to nine hours of sleep nightly for optimal health. Chronic sleep deprivation affects nearly every body system. Prioritizing adequate sleep supports cancer prevention along with numerous other health benefits. Good sleep hygiene practices promote better sleep quality.
Chronic psychological stress may influence cancer development and progression, though mechanisms are complex. Stress affects immune function and promotes unhealthy coping behaviors including smoking, excessive alcohol consumption, and poor diet. Managing stress through healthy strategies supports overall cancer prevention efforts.
Habits That Can Significantly Reduce Your Cancer Risk

Adopting specific habits substantially reduces cancer risk. Research demonstrates that lifestyle modifications can prevent a significant proportion of cancer cases. These habits work synergistically, with combined effects exceeding individual impacts. Starting today with even small changes provides meaningful protection.
The beauty of cancer prevention through lifestyle is that the same habits that reduce cancer risk also prevent heart disease, diabetes, and other chronic conditions. These behaviors promote overall health, vitality, and longevity. Investing in healthy habits pays lifelong dividends.
Maintain Tobacco-Free Status Throughout Life
Never starting tobacco use represents the single most important cancer prevention decision. For current smokers, quitting provides substantial benefits regardless of age or smoking duration. The body begins healing immediately after the last cigarette.
Within weeks of quitting, lung function improves and circulation gets better. Within months, coughing and shortness of breath decrease. Within one year, heart attack risk drops by half. After five to ten years, lung cancer risk decreases significantly. After 15 years, heart disease risk approaches that of never-smokers.
Quitting smoking is challenging due to nicotine addiction. However, numerous effective cessation aids exist. Nicotine replacement therapy, prescription medications, behavioral counseling, and support groups all improve quit success rates. Most successful ex-smokers required multiple quit attempts before achieving long-term abstinence.
Avoid secondhand smoke exposure. Make your home and car smoke-free. Support smoke-free workplace policies. Protecting yourself and others from tobacco smoke benefits everyone’s health. Choose smoke-free venues when possible.

Achieve and Maintain Healthy Body Weight
Maintaining healthy body weight throughout life significantly reduces cancer risk. For people who are overweight or obese, even modest weight loss provides benefits. The goal is gradual, sustainable weight management through balanced eating and regular physical activity.
Focus on behaviors rather than rapid weight loss. Crash diets rarely produce lasting results and may harm health. Instead, develop sustainable eating patterns you can maintain long-term. Small, consistent changes accumulate over time to produce meaningful results.
Monitor your weight regularly and act when it starts creeping up. Weight gain often occurs gradually, making it easy to ignore. Addressing small gains immediately prevents larger weight increases. Most adults gain one to two pounds annually, which adds up over decades.
Remember that body composition matters beyond just weight. Muscle tissue is denser than fat. Strength training builds muscle while reducing fat. The scale may not reflect these positive changes. How your clothes fit and your overall energy level provide additional measures of progress.
Engage in Regular Physical Activity
Physical activity represents one of the most powerful cancer prevention strategies. Exercise reduces risk for colon, breast, endometrial, kidney, bladder, esophageal, and stomach cancers. The protective effects work through multiple mechanisms including weight management, hormone regulation, immune enhancement, and inflammation reduction.
The American Cancer Society recommends at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous-intensity activity weekly. Moderate-intensity activities include brisk walking, recreational swimming, and doubles tennis. Vigorous activities include jogging, fast cycling, and lap swimming.
Muscle-strengthening activities should be performed at least twice weekly. Strength training builds and maintains muscle mass, which supports healthy metabolism. As we age, maintaining muscle becomes increasingly important. Resistance exercises can be performed with weights, resistance bands, or body weight.
Find activities you enjoy to ensure consistency. Walking is accessible, free, and suitable for most people. Dancing, gardening, recreational sports, and active play with children or grandchildren all count. The best exercise is the one you’ll actually do regularly.
Starting Small: If you’re currently inactive, start with just 10 minutes of activity daily and gradually increase. Even small amounts of physical activity provide benefits. Every step counts toward reducing cancer risk. Breaking activity into shorter sessions throughout the day works as well as single longer sessions.

Adopt a Plant-Forward Eating Pattern
A dietary pattern rich in plant-based foods provides powerful cancer protection. Vegetables, fruits, whole grains, legumes, nuts, and seeds contain thousands of beneficial compounds including fiber, vitamins, minerals, and phytochemicals that reduce cancer risk through multiple mechanisms.
Fill at least two-thirds of your plate with plant foods at each meal. Choose colorful vegetables and fruits to maximize nutrient diversity. Different colors provide different protective compounds. Aim for variety across days and weeks.
Whole grains provide fiber and numerous other beneficial compounds refined grains lack. Choose whole wheat bread, brown rice, quinoa, oats, and other whole grains over white bread, white rice, and other refined grain products. Read labels—”whole grain” should appear as the first ingredient.
Legumes including beans, lentils, and peas offer plant-based protein, fiber, and numerous cancer-protective compounds. These versatile foods work in soups, salads, side dishes, and main courses. Replacing some animal protein with legumes benefits health and the environment.
Cancer-Protective Foods to Emphasize
- Colorful vegetables of all types
- Fresh and frozen fruits
- Whole grain breads and cereals
- Beans, lentils, and peas
- Nuts and seeds
- Green tea
- Herbs and spices like turmeric
- Garlic and onions
- Cruciferous vegetables like broccoli
- Tomatoes and tomato products
Practical Dietary Strategies
- Make half your plate vegetables
- Choose whole fruits over juice
- Replace refined grains with whole grains
- Include legumes several times weekly
- Limit red meat to occasional consumption
- Avoid processed meats entirely
- Cook at home more often
- Read ingredient labels carefully
- Stay hydrated with water
- Practice mindful portion control

Limit or Eliminate Alcohol Consumption
Given alcohol’s established link to multiple cancers, limiting consumption reduces risk. If you don’t drink, don’t start. The potential cardiovascular benefits of moderate drinking do not outweigh cancer risks for most people. If you choose to drink, strict moderation is essential.
For cancer prevention, less is better when it comes to alcohol. Many cancer prevention experts recommend avoiding alcohol entirely. If you drink, limit consumption to no more than one drink daily for women or two for men. One drink equals 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits.
Women should be particularly mindful of alcohol’s breast cancer risk. Even light drinking modestly increases risk. Women with family history of breast cancer or other risk factors should consider avoiding alcohol completely. Discuss your individual situation with your healthcare provider.
Practice Sun Safety and Protect Your Skin
Protecting skin from excessive ultraviolet radiation prevents most skin cancers. Sun protection should begin in childhood and continue throughout life. Cumulative sun exposure over decades increases skin cancer risk, but it’s never too late to start protecting yourself.
Apply broad-spectrum sunscreen with SPF 30 or higher to exposed skin before going outdoors. Reapply every two hours and after swimming or sweating. Sunscreen should complement, not replace, other sun protection strategies. No sunscreen blocks 100 percent of UV rays.
Seek shade during peak sun intensity hours between 10 AM and 4 PM when UV radiation is strongest. Plan outdoor activities for early morning or late afternoon when possible. When outside during peak hours, find shaded areas under trees, umbrellas, or structures.
Wear sun-protective clothing including long-sleeved shirts, pants, and wide-brimmed hats. Special UV-protective clothing provides excellent sun protection. Regular clothing also protects, with darker colors and tighter weaves offering more protection. Cover as much skin as practical.
Never use tanning beds or sun lamps. These devices emit UV radiation that increases skin cancer risk dramatically. There is no safe indoor tanning. The temporary tan is not worth the long-term cancer risk. Self-tanning products provide a safer alternative for those desiring darker skin tone.

Get Vaccinated Against Cancer-Causing Infections
Vaccines prevent infections that cause cancer. The HPV vaccine protects against human papillomavirus types that cause cervical, anal, throat, and other cancers. HPV vaccination is recommended for children around age 11 or 12, but can be given through age 45 for those not previously vaccinated.
The hepatitis B vaccine prevents infection that can lead to liver cancer. Hepatitis B vaccination is now routine for infants, but many adults were not vaccinated. Adults at risk for hepatitis B exposure should discuss vaccination with their healthcare provider. This includes healthcare workers, people with multiple sexual partners, and those with certain medical conditions.
These vaccines are safe and highly effective. They provide long-lasting protection against cancer-causing infections. Getting vaccinated protects both yourself and others through reduced disease transmission. Vaccination represents a simple, one-time or limited-series action with lifelong benefits.
Participate in Recommended Cancer Screenings
While screening is detection rather than prevention, it prevents cancer deaths and some screenings prevent cancer itself. Following screening guidelines appropriate for your age and risk factors represents a crucial cancer risk reduction strategy. Many Americans skip recommended screenings, missing opportunities for early detection.
Colonoscopy screening prevents colorectal cancer by identifying and removing precancerous polyps. Current guidelines recommend beginning screening at age 45 for average-risk individuals. Colonoscopy every 10 years represents one option; other screening methods exist. People with family history or other risk factors may need earlier or more frequent screening.
Mammography screening detects breast cancer at early, highly treatable stages. Guidelines vary slightly among organizations, but generally recommend beginning mammography between ages 40-50 for average-risk women. Annual or biennial screening is recommended depending on individual risk factors. Discuss appropriate timing with your healthcare provider.
Cervical cancer screening through Pap tests and HPV testing prevents cervical cancer through early detection of precancerous changes. Screening typically begins at age 21 and continues through age 65 with appropriate frequency based on results. Cervical cancer rates have declined dramatically due to screening.
Lung cancer screening with low-dose CT scan benefits current and former heavy smokers aged 50 to 80 years. Eligibility criteria include smoking history of at least 20 pack-years. Lung cancer screening can detect cancer at early stages when surgical cure is possible. Discuss screening with your doctor if you meet criteria.
| Screening Test | Cancer Type | Who Should Be Screened | Frequency |
| Colonoscopy | Colorectal | Adults age 45-75 | Every 10 years |
| Mammography | Breast | Women age 40-74 | Annual or biennial |
| Pap Test/HPV Test | Cervical | Women age 21-65 | Every 3-5 years |
| Low-Dose CT Scan | Lung | Heavy smokers age 50-80 | Annually |
| PSA Test | Prostate | Men age 55-69 (discuss with doctor) | Individualized |
Know Your Family History and Personal Risk
Understanding your family cancer history helps identify elevated risk requiring enhanced surveillance or preventive interventions. Some people inherit genetic mutations that substantially increase cancer risk. Genetic counseling and testing may be appropriate for those with strong family histories.
Compile a detailed family medical history including cancers in first-degree relatives (parents, siblings, children) and second-degree relatives (grandparents, aunts, uncles, nieces, nephews). Note the type of cancer and age at diagnosis. Multiple relatives with the same or related cancers suggest possible hereditary syndrome.
Discuss your family history with your healthcare provider. Enhanced screening, preventive medications, or other interventions may be recommended based on elevated risk. People with hereditary cancer syndromes may benefit from genetic counseling and testing to guide prevention and screening strategies.

Manage Stress and Prioritize Mental Health
While direct links between stress and cancer development remain under investigation, chronic stress promotes unhealthy behaviors that increase cancer risk. Stress management supports overall health and facilitates maintenance of healthy habits. Mental health is inseparable from physical health.
Develop healthy stress management strategies that work for you. Regular physical activity reduces stress and anxiety. Mindfulness meditation shows benefits for stress reduction. Deep breathing exercises provide quick stress relief. Spending time in nature improves mood and reduces stress hormones.
Maintain strong social connections. Relationships provide emotional support and buffer against stress. Loneliness and social isolation harm health. Invest time in relationships with family and friends. Join clubs, groups, or community organizations aligned with your interests.
Seek professional help when needed. Mental health conditions including depression and anxiety are treatable. Therapy provides tools for managing stress and improving coping skills. Medication may be appropriate for some people. Don’t hesitate to ask for help—it’s a sign of strength, not weakness.
Get Adequate Quality Sleep
Prioritizing adequate sleep supports numerous aspects of health including immune function, hormone regulation, and DNA repair—all relevant to cancer prevention. Most adults need seven to nine hours of sleep nightly. Chronic sleep deprivation accumulates as sleep debt that affects health.
Establish consistent sleep and wake times, even on weekends. Your body’s circadian rhythm functions best with regular schedules. Create a relaxing bedtime routine that signals your body to prepare for sleep. Avoid screens for at least 30 minutes before bed, as blue light suppresses melatonin.
Optimize your sleep environment. Keep your bedroom cool, dark, and quiet. Use blackout curtains if needed. Consider white noise machines if environmental noise disrupts sleep. Invest in a comfortable mattress and pillows. Reserve your bedroom for sleep and intimacy, not work or entertainment.
Avoid caffeine in the afternoon and evening. Limit alcohol, which may help you fall asleep but disrupts sleep quality. Regular physical activity improves sleep, but avoid vigorous exercise close to bedtime. If you struggle with persistent sleep problems, discuss with your healthcare provider. Sleep disorders are treatable.
Taking Action: Your Path Forward in Cancer Prevention

Cancer in the USA represents a significant health challenge affecting millions of Americans each year. However, this comprehensive exploration reveals that we are not powerless against this disease. Understanding cancer’s scope, causes, and prevention strategies empowers each person to take meaningful protective action.
The statistics are sobering—nearly 2 million new cancer cases diagnosed annually and over 600,000 deaths. Yet these numbers also tell a story of progress. Death rates have declined by approximately 33 percent since peaking in the early 1990s. This represents millions of lives saved through prevention, early detection, and improved treatment.
Cancer affects all age groups, with risk increasing dramatically after age 50. The disease creates profound stress for patients and families through emotional, physical, and financial burdens. However, treatment effectiveness has improved remarkably. Many cancers are now curable when detected early, and others have become manageable chronic conditions.
Key Takeaways for Cancer Prevention
Prevention offers the most powerful tool against cancer. Approximately 40 percent of cancer cases are associated with modifiable risk factors. Lifestyle choices accumulated over decades significantly influence cancer risk. The good news is that you control these choices.
Tobacco use remains the leading preventable cause of cancer. Maintaining healthy weight, engaging in regular physical activity, and eating a plant-forward diet substantially reduce risk. Limiting alcohol, practicing sun safety, getting vaccinated against cancer-causing infections, and participating in recommended screenings all contribute to protection.
These habits work together synergistically. You don’t need to be perfect—even modest improvements provide meaningful benefits. Starting today, regardless of your age or current health status, you can take steps that reduce your cancer risk and improve your overall health.
Remember: Small changes maintained over time create substantial health benefits. You don’t need to overhaul your entire life overnight. Choose one or two areas where you can make improvements and build from there. Progress, not perfection, is the goal.
Moving Forward With Knowledge and Hope
Understanding cancer as both a preventable and increasingly treatable disease allows for informed decision-making. Knowledge empowers action. The information in this comprehensive guide provides a foundation for protecting yourself and your loved ones.
Medical research continues advancing rapidly. New prevention strategies, screening technologies, and treatments emerge regularly. Stay informed about cancer prevention through reliable sources. Discuss your individual risk factors and appropriate preventive measures with your healthcare provider.
Support cancer research and public health initiatives that benefit everyone. Advocate for policies promoting cancer prevention including tobacco control, environmental protection, and equitable healthcare access. Individual actions matter, but collective efforts amplify impact.
If you receive a cancer diagnosis, remember that many cancers are treatable and even curable, especially when detected early. Seek care from experienced oncology teams, explore all treatment options including clinical trials, and utilize available support services. You are not alone in facing this challenge.
Immediate Actions You Can Take
- Schedule any overdue cancer screenings
- Quit tobacco or avoid starting
- Increase daily physical activity
- Add more vegetables to your meals
- Practice sun protection
- Limit alcohol consumption
- Discuss HPV and hepatitis B vaccination
- Compile your family medical history
- Reduce processed food consumption
- Prioritize adequate sleep
Resources for Continued Learning
- American Cancer Society (cancer.org)
- National Cancer Institute (cancer.gov)
- Centers for Disease Control (cdc.gov/cancer)
- Cancer research organizations
- Local cancer support groups
- Healthcare provider guidance
- Reputable medical websites
- Cancer prevention programs
- Nutrition and lifestyle counseling
- Genetic counseling services
Cancer prevention is a lifelong journey, not a destination. Each day presents opportunities to make choices that protect your health. The habits you establish today will benefit you for years and decades to come. Your choices also influence those around you, particularly children who learn from your example.
Take inspiration from the progress already achieved against cancer. Science continues advancing. Early detection continues improving. Treatment continues getting more effective. Many people survive cancer and return to full, active lives. The future of cancer prevention and treatment holds great promise.

Your health is your most valuable asset. Investing time and effort in cancer prevention pays dividends throughout your life. Start where you are, use what you have, do what you can. Every step forward, no matter how small, contributes to reducing your cancer risk and improving your overall wellbeing.
Share this knowledge with family and friends. Prevention benefits everyone. By working together as individuals, families, communities, and a nation, we can reduce the burden of cancer in the USA and save countless lives. The power to prevent cancer lies within each of us.