Heart Disease in the USA: A Century of America’s Leading Killer
Heart disease has maintained its grim status as the number one cause of death in the United States for over a century. Every 34 seconds, someone in America dies from cardiovascular disease, claiming more lives annually than all forms of cancer and accidents combined. Despite medical advances, heart disease continues to affect nearly half of all American adults. This article explores how heart disease rose to become America’s deadliest health threat, why it persists despite being largely preventable, and what can be done to change this troubling trajectory.
Heart Disease in the USA: The Alarming Numbers
Heart disease remains the leading cause of death in the United States, accounting for approximately 1 in 4 deaths annually.
According to the Centers for Disease Control and Prevention (CDC), heart disease claims approximately 697,000 American lives each year. That’s one death every 34 seconds. In 2023 alone, there were 915,973 total deaths from cardiovascular disease, including heart disease, stroke, hypertension, and heart failure.
The American Heart Association’s 2025 Heart Disease and Stroke Statistics Update reveals that heart disease has been the leading cause of death in the U.S. for more than a century. While medical advances have helped more people live longer with cardiovascular diseases, many risk factors continue to grow at alarming rates:
- Nearly 47% of U.S. adults have high blood pressure
- More than 72% of U.S. adults have unhealthy weight, with nearly 42% having obesity
- More than half of U.S. adults (57%) have type 2 diabetes or prediabetes
- Cardiovascular diseases, including heart disease and stroke, claim more lives in the U.S. than all forms of cancer and accidental deaths – the #2 and #3 causes of death – combined
These statistics paint a sobering picture of America’s heart health crisis. But to understand how we arrived here, we must look back at the historical shift in America’s leading causes of death.
The 100-Year Rise: How Heart Disease Became America’s #1 Killer
At the beginning of the 20th century, infectious diseases like pneumonia, tuberculosis, and gastrointestinal infections were the leading causes of death in America. The transition to heart disease as the primary killer represents one of the most significant epidemiological shifts in modern history.
This transformation began around the 1920s and accelerated after World War II, coinciding with several major societal changes:
Urbanization & Industrialization
As Americans moved from farms to cities, physical activity decreased dramatically. Jobs shifted from manual labor to sedentary office work, reducing daily caloric expenditure.
Dietary Revolution
The post-WWII era saw the rise of processed foods, fast food chains, and convenience meals high in saturated fats, sodium, and refined sugars—all contributors to heart disease.
Tobacco Usage
Cigarette smoking became widespread in the mid-20th century, significantly increasing heart disease risk before its dangers were fully understood.
By the 1950s, heart disease had firmly established itself as America’s number one killer. The American Heart Association, founded in 1924, began its transformation from a professional scientific society to a voluntary health organization fighting cardiovascular disease.
Medical advances in the latter half of the 20th century, including bypass surgery, statins, and better emergency response systems, helped reduce heart disease mortality rates. However, these improvements have been offset by the continuing rise in risk factors like obesity and diabetes, keeping heart disease firmly in the top position.
The Perfect Storm: Why Heart Disease Thrives in Modern America
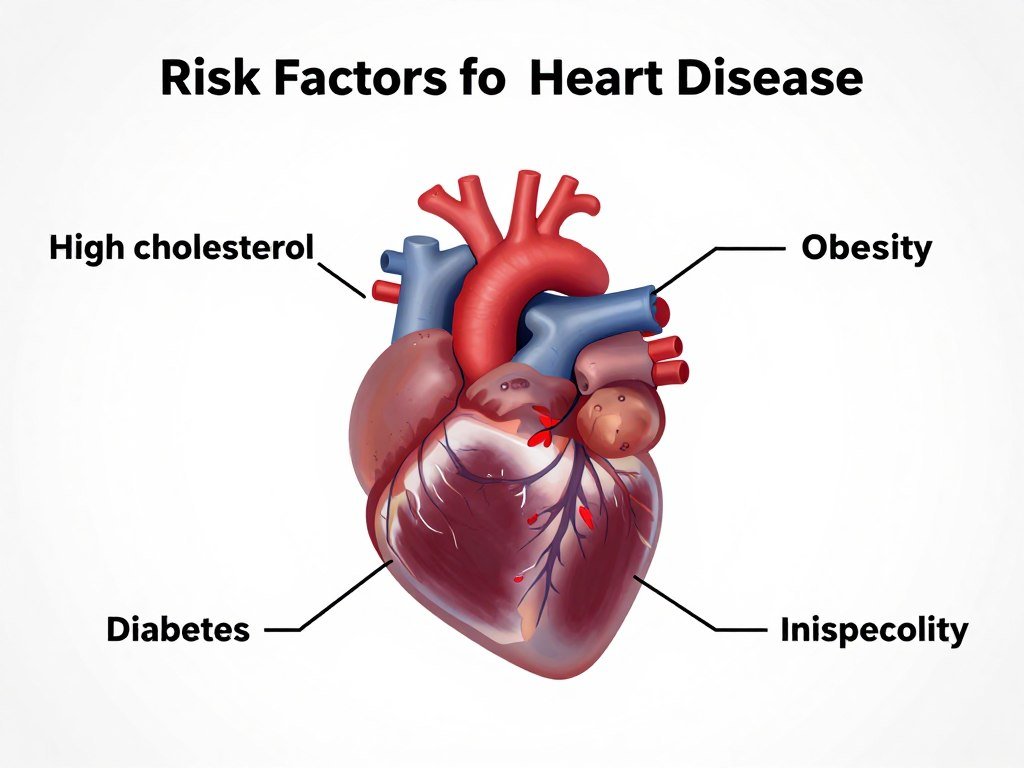
Multiple interconnected risk factors contribute to the high prevalence of heart disease in the United States.
The persistence of heart disease as America’s leading killer stems from a complex interplay of modifiable and non-modifiable risk factors. Understanding these factors is crucial to addressing the epidemic.
Modifiable Risk Factors
Dietary Patterns
The typical American diet is characterized by high consumption of processed foods, saturated fats, added sugars, and sodium—all linked to increased heart disease risk. According to the Dietary Guidelines for Americans, most Americans consume far more sodium and saturated fat than recommended.
Physical Inactivity
Only about 25% of U.S. adults meet the recommended physical activity guidelines. Sedentary lifestyles contribute significantly to heart disease risk by affecting weight, blood pressure, and overall cardiovascular health.
Tobacco Use
Despite declining rates, smoking remains a major contributor to heart disease, responsible for about 1 in 4 heart disease deaths. E-cigarette use has emerged as a new concern, especially among youth.
Obesity Epidemic
More than 40% of American adults have obesity, a major risk factor for heart disease. The CDC reports that obesity rates have increased dramatically over the past few decades.
Medical Risk Factors
High Blood Pressure
Nearly half of American adults have hypertension, often called the “silent killer” because it typically has no symptoms but significantly increases heart disease risk.
High Cholesterol
About 38% of American adults have high cholesterol levels, which can lead to atherosclerosis and increased risk of heart attack and stroke.
Diabetes
More than 37 million Americans have diabetes, which doubles or quadruples the risk of heart disease. Another 96 million have prediabetes.
Socioeconomic and Demographic Factors
Heart disease doesn’t affect all Americans equally. Significant disparities exist based on race, ethnicity, gender, and socioeconomic status:
- Black Americans have higher rates of hypertension and heart disease mortality than white Americans
- Women are less likely to receive prompt diagnosis and treatment for heart attacks
- Lower-income communities often have limited access to healthy foods and safe places for physical activity
- Rural areas frequently have fewer healthcare resources for prevention and treatment
These disparities highlight the complex social determinants that contribute to heart disease risk beyond individual behaviors.
The American Diet: Fuel for a Heart Disease Epidemic

Diet plays a crucial role in heart disease risk, with plant-based and whole foods offering protection while processed foods increase risk.
Diet is perhaps the most significant modifiable risk factor for heart disease. The evolution of the American diet over the past century closely parallels the rise of heart disease as the leading cause of death.
Foods That Harm Heart Health
| Food Category | Examples | Heart Health Impact |
| Processed Meats | Bacon, sausage, hot dogs, deli meats | High in sodium and preservatives; associated with 42% higher risk of heart disease |
| Trans Fats | Some margarines, fried fast foods, commercially baked goods | Raise LDL (“bad”) cholesterol while lowering HDL (“good”) cholesterol |
| Sugary Beverages | Soda, sweetened tea, sports drinks, fruit juices | Linked to obesity, type 2 diabetes, and increased heart disease risk |
| Refined Carbohydrates | White bread, pastries, white rice, many breakfast cereals | Spike blood sugar, contribute to inflammation and obesity |
| High-Sodium Foods | Canned soups, frozen meals, snack foods, restaurant meals | Increase blood pressure, a major risk factor for heart disease |
Heart-Protective Foods
Research consistently shows that certain dietary patterns and foods can significantly reduce heart disease risk:
Mediterranean Diet
Rich in olive oil, nuts, fish, fruits, vegetables, and whole grains, this diet has been shown to reduce heart disease risk by up to 30% according to the PREDIMED study.
DASH Diet
Designed to fight hypertension, the Dietary Approaches to Stop Hypertension diet emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while limiting sodium.
Plant-Based Diets
Vegetarian and vegan diets are associated with lower blood pressure, cholesterol levels, and heart disease risk when properly planned.
The American Heart Association recommends limiting saturated fat to less than 6% of daily calories, minimizing trans fats, reducing sodium to less than 2,300mg daily, and limiting added sugars to no more than 6 teaspoons for women and 9 teaspoons for men.
Preventing Heart Disease: Strategies That Work
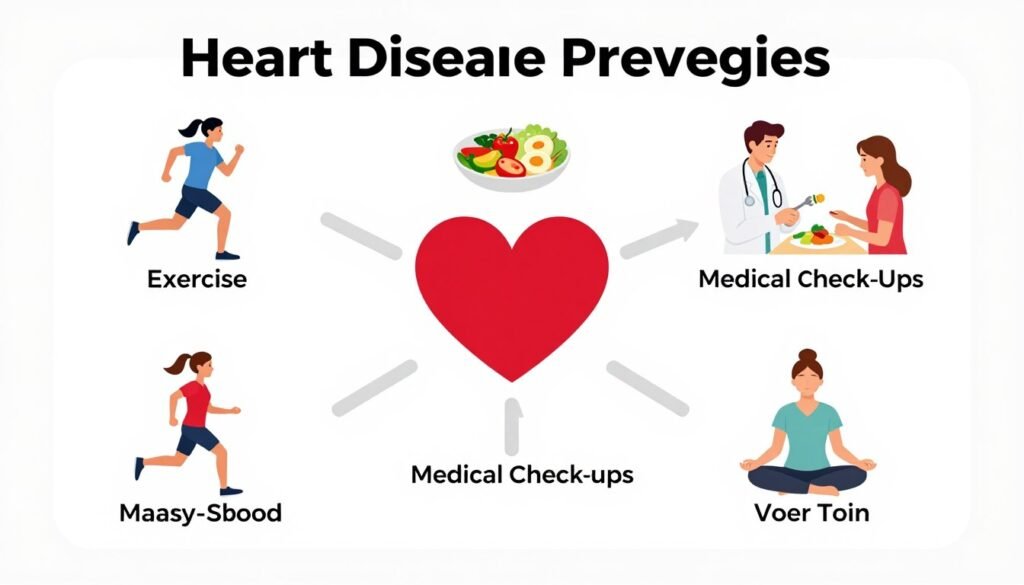
A comprehensive approach to heart disease prevention includes lifestyle modifications, regular screenings, and medical management when necessary.
Despite the alarming statistics, heart disease is largely preventable. The American Heart Association’s Life’s Essential 8 framework identifies key measures for improving and maintaining cardiovascular health:
Eat Better
Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting processed foods, sodium, and added sugars.
Be More Active
Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity weekly.
Quit Tobacco
Smoking cessation rapidly reduces heart disease risk, with benefits beginning within hours of quitting.
Get Healthy Sleep
Adults should aim for 7-9 hours of quality sleep per night to support heart health.
Manage Weight
Maintaining a healthy weight through diet and exercise significantly reduces heart disease risk.
Control Cholesterol
Regular screening and management through diet, exercise, and medication when necessary.
Manage Blood Sugar
Preventing or controlling diabetes through lifestyle modifications and appropriate medical care.
Manage Blood Pressure
Regular monitoring and control through diet, exercise, stress management, and medication if needed.
Public Health Approaches
Individual efforts must be supported by broader public health initiatives:
- Policy changes to reduce sodium and trans fats in the food supply
- Urban planning that promotes physical activity through walkable communities
- Workplace wellness programs that support heart-healthy behaviors
- School-based interventions to establish healthy habits early in life
- Public education campaigns about heart disease risk factors and warning signs
Studies show that comprehensive prevention strategies could prevent up to 80% of premature heart disease deaths. According to research published in the Journal of the American Heart Association, optimal adherence to Life’s Essential 8 measures is associated with a 74% lower risk of cardiovascular events compared to poor adherence.
The Perception Gap: Why Aren’t We More Concerned?
Despite being America’s leading killer, heart disease often doesn’t receive the public attention and concern it warrants.
Given that heart disease has been America’s leading killer for over a century, why isn’t there greater public concern and action? Several factors contribute to this perception gap:
The “Slow Burn” Nature
Unlike infectious diseases or cancer, heart disease typically develops gradually over decades. This slow progression makes it easier to ignore or postpone preventive action. The absence of symptoms until late stages further contributes to complacency.
Normalization of Risk Factors
Many heart disease risk factors—obesity, sedentary lifestyle, poor diet—have become normalized in American society. When unhealthy behaviors are common, they’re perceived as less threatening despite their dangers.
Competing Health Concerns
Media coverage often focuses on more novel or dramatic health threats. Cancer, for example, receives significantly more research funding relative to its mortality burden compared to heart disease.
Prevention Complexity
Heart disease prevention requires sustained lifestyle changes across multiple domains—diet, exercise, stress management—rather than a single intervention like a vaccine. This complexity makes prevention seem more daunting.
Optimism Bias
Many people underestimate their personal risk of heart disease, believing that it affects “others” but not themselves. This optimism bias reduces motivation for preventive behaviors.
Addressing this perception gap requires better public education about heart disease risk, symptoms (which differ between men and women), and the effectiveness of prevention strategies. Making the invisible visible—through risk calculators, regular screenings, and clear communication—can help bridge this gap.
The Future of Heart Disease in America

Emerging technologies and treatments offer hope for reducing the burden of heart disease, though challenges remain.
What does the future hold for heart disease in America? Projections and emerging trends paint a mixed picture:
Concerning Trends
Several factors suggest heart disease will remain a significant health challenge:
- Rising obesity rates among youth, potentially creating a new generation with elevated heart disease risk
- Increasing prevalence of diabetes, particularly among younger adults
- Persistent socioeconomic and racial disparities in heart disease risk and outcomes
- Climate change impacts on physical activity, food systems, and air quality that may affect cardiovascular health
Promising Developments
However, several advances offer hope for reducing heart disease burden:
Medical Innovations
New medications like PCSK9 inhibitors and GLP-1 receptor agonists show promise for managing cholesterol and weight. Advances in minimally invasive procedures continue to improve treatment outcomes.
Precision Medicine
Genetic testing and personalized risk assessment allow for more targeted prevention and treatment strategies tailored to individual risk profiles.
Digital Health
Wearable devices, telemedicine, and mobile health applications are expanding access to monitoring and care while enabling earlier intervention.
According to projections from the American Heart Association, if current trends continue, by 2035 more than 45% of Americans will have some form of cardiovascular disease, with total costs reaching $1.1 trillion annually.
However, research suggests that implementing comprehensive prevention strategies could prevent up to 80% of premature heart disease deaths. The future trajectory of heart disease in America will largely depend on our collective commitment to prevention, equity, and innovation.
Conclusion: Changing the Heart Disease Narrative

Through collective action and individual choices, we can change the trajectory of heart disease in America.
Heart disease has maintained its position as America’s leading killer for over a century, but this doesn’t mean it must remain so. Unlike many health threats, heart disease is largely preventable through lifestyle modifications and appropriate medical care.
The story of heart disease in America reflects broader societal changes—urbanization, industrialization, food system transformation, and technological advancement. Addressing this epidemic requires equally broad responses that span individual choices, healthcare practices, public policy, and cultural norms.
By understanding the historical rise of heart disease, recognizing current risk factors, implementing evidence-based prevention strategies, and leveraging emerging technologies, we can work toward a future where heart disease no longer claims its current toll of American lives.
The path forward requires commitment at all levels—from individuals making daily choices about diet and physical activity to policymakers shaping food systems and healthcare access. With concerted effort, heart disease need not remain America’s leading killer for another century.
For more information on heart disease prevention and management, visit the American Heart Association or the Centers for Disease Control and Prevention.