Tobacco Use Health Threat USA: Understanding the Crisis and Finding Solutions
Tobacco use remains one of the most significant preventable health threats in the United States. Despite decades of public health campaigns, millions of Americans continue to smoke cigarettes and use tobacco products daily. This comprehensive guide explores why tobacco use health threat USA matters, how addiction develops, and what evidence-based solutions can help.
Every year, tobacco-related diseases claim hundreds of thousands of lives across the nation. Understanding the scope of this crisis is the first step toward meaningful change.
Why Smoking and Tobacco Use Is a Major Threat to US Health
Tobacco use stands as the leading preventable cause of disease and death in the United States. The health consequences of smoking tobacco extend far beyond the individual smoker, affecting families, communities, and the entire healthcare system.
Cigarette smoking causes approximately 480,000 deaths annually among adults in the United States. This staggering number represents nearly one in five deaths each year. The chemicals in tobacco smoke damage nearly every organ in the body, leading to serious diseases and reducing overall health quality.
The economic burden is equally devastating. Healthcare costs related to smoking exceed $170 billion annually, while lost productivity adds another $156 billion to the national economic toll. These figures demonstrate that tobacco use health threat USA extends beyond individual health to impact society broadly.
Important Health Fact: Smoking tobacco increases the risk of coronary heart disease by two to four times and stroke by two to four times compared to non-smokers.
Primary Health Consequences of Tobacco Use
Respiratory Diseases
Cigarette smoke damages lung tissue and airways, leading to chronic conditions that severely limit breathing capacity and quality of life.
- Chronic obstructive pulmonary disease (COPD)
- Emphysema and chronic bronchitis
- Increased susceptibility to respiratory infections
- Reduced lung function over time
Cardiovascular Diseases
Tobacco use significantly elevates risk for various heart and blood vessel conditions that can prove fatal.
- Heart disease and heart attacks
- Stroke and peripheral vascular disease
- Elevated blood pressure and heart rate
- Damaged blood vessel walls
Cancer Development
Smoking causes cancer in multiple body systems, with lung cancer being the most common tobacco-related malignancy.
- Lung cancer (leading cause among adults)
- Throat, mouth, and esophageal cancers
- Bladder, kidney, and pancreatic cancers
- Cervical and stomach cancers
Other Health Effects
Beyond major diseases, tobacco use damages reproductive health, bones, eyes, and immune function throughout the body.
- Type 2 diabetes complications
- Reproductive health problems
- Weakened immune system response
- Vision problems and blindness risk
Ready to Take Action? Free quit smoking resources are available through the Centers for Disease Control and Prevention and the American Lung Association. These evidence-based programs have helped millions quit successfully.
Secondhand Smoke Impact
The health threat extends beyond people who smoke. Secondhand smoke exposure causes approximately 41,000 deaths among non-smoking adults each year in the United States. Children exposed to tobacco smoke face increased risks for sudden infant death syndrome, acute respiratory infections, ear problems, and more severe asthma attacks.
No level of secondhand smoke exposure is safe. Even brief exposure can damage the cardiovascular system and interfere with normal blood vessel function. This reality makes tobacco use a public health concern that affects entire communities.
Understanding Tobacco Addiction: Definition and Mechanisms
Tobacco addiction is a chronic condition characterized by compulsive tobacco use despite harmful consequences. The primary addictive substance in tobacco products is nicotine, a powerful chemical that alters brain function and creates physical dependence.
When someone inhales cigarette smoke, nicotine reaches the brain within seconds. This rapid delivery creates an immediate effect on the brain’s reward system, releasing dopamine and other neurotransmitters that produce pleasurable sensations. Over time, the brain adapts to regular nicotine exposure and requires the substance to function normally.
How Nicotine Addiction Develops
Nicotine addiction involves both physical and psychological components. The physical addiction occurs as brain chemistry changes in response to repeated nicotine exposure. Nicotine receptors in the brain multiply, requiring more nicotine to achieve the same effect. This tolerance drives increased tobacco use over time.
Physical Addiction Factors
- Rapid nicotine absorption through lung tissue
- Altered brain receptor sensitivity and number
- Withdrawal symptoms upon cessation
- Tolerance requiring increased consumption
- Chemical dependence affecting multiple body systems
Psychological Addiction Elements
- Behavioral associations with smoking routines
- Emotional regulation through nicotine use
- Social connections related to tobacco use
- Stress management habits involving cigarettes
- Identity and self-perception tied to smoking
The psychological aspects of tobacco addiction are equally powerful. People smoke in response to specific triggers, situations, emotions, or times of day. These learned behaviors become deeply ingrained habits that reinforce the addiction beyond the physical need for nicotine.
“Nicotine is as addictive as heroin or cocaine, making it extremely difficult to quit without support and treatment.”
National Quit Helpline Available 24/7
Trained counselors can help you understand your addiction and create a personalized quit plan. Free support is just a phone call away.
Chemicals in Tobacco Smoke
While nicotine drives addiction, cigarette smoke contains over 7,000 chemicals. At least 70 of these chemicals are known to cause cancer. These harmful substances include tar, carbon monoxide, formaldehyde, ammonia, hydrogen cyanide, arsenic, and DDT.
Each time someone smokes a cigarette, these toxic chemicals enter the bloodstream and spread throughout the body. The cumulative exposure over years of smoking tobacco creates the severe health consequences associated with tobacco use.
Age Groups Most Affected by Tobacco Use in the USA
Tobacco use affects Americans across all age groups, but certain populations face higher risks and prevalence rates. Understanding these patterns helps target prevention and cessation efforts effectively.
Young Adults and Tobacco Initiation
Young adults aged 18 to 25 years represent a critical demographic for tobacco use intervention. Approximately 90% of adult smokers began smoking before age 18, with 99% starting by age 26. This pattern makes young adulthood a crucial period for both prevention and early cessation efforts.
Among adults, the highest smoking rates occur in people aged 25 to 44 years. Nearly 17% of adults in this age bracket currently smoke cigarettes. This group faces particular challenges because they are in prime working years, often balancing career demands, family responsibilities, and financial pressures that can make quitting more difficult.
| Age Group | Current Smoking Rate | Primary Tobacco Products Used | Key Challenges |
| 18-24 years | 10.8% | Cigarettes, e-cigarettes, hookah | Social influence, stress, experimentation |
| 25-44 years | 16.7% | Cigarettes, smokeless tobacco | Work stress, established habits, time constraints |
| 45-64 years | 15.5% | Cigarettes | Long-term addiction, health concerns emerging |
| 65+ years | 8.3% | Cigarettes | Chronic diseases, decades-long addiction |
Middle-Aged Adults and Long-Term Use
Adults aged 45 to 64 years show smoking rates around 15.5%. Many people in this age group have smoked for decades, making their addiction deeply entrenched. However, this is also the age when smoking-related health problems often begin to manifest, creating strong motivation to quit.
This age group benefits significantly from cessation efforts. Even after years of smoking tobacco, quitting can substantially reduce disease risk and improve health outcomes. Research shows that people who quit smoking before age 50 cut their risk of dying in the next 15 years in half compared to those who continue.
Older Adults and Health Consequences
Among adults aged 65 and older, smoking rates drop to about 8.3%. Lower rates in older adults partly reflect the harsh reality that many long-term smokers die prematurely from tobacco-related diseases. Survivors often quit due to serious health problems or medical advice.
For older adults who still smoke, quitting remains beneficial. Even at advanced ages, cessation improves cardiovascular function, reduces cancer risk, and enhances overall quality of life. Healthcare providers emphasize that it is never too late to quit smoking.
Youth E-Cigarette Crisis: While traditional cigarette smoking has declined among youth, e-cigarette use has surged. In recent years, over 20% of high school students reported using e-cigarettes, creating a new generation at risk for nicotine addiction.
Targeted resources exist for different age groups. Young adults benefit from peer support programs and digital cessation tools. Middle-aged adults often respond well to counseling combined with cessation medications. Older adults may need specialized approaches that address multiple health conditions simultaneously.
How Tobacco Use Becomes Stressful and Out of Control in the USA

What often begins as casual or social smoking quickly spirals into a powerful addiction that controls daily life. The progression from occasional tobacco use to compulsive dependency creates significant stress for individuals and their families.
The Addiction Cycle
Tobacco addiction creates a vicious cycle that becomes increasingly difficult to escape. As tolerance develops, smokers need more cigarettes to satisfy cravings. Between cigarettes, withdrawal symptoms emerge, including irritability, anxiety, difficulty concentrating, and intense cravings. These unpleasant symptoms drive the next cigarette, perpetuating the cycle.
The loss of control manifests in several ways. Many smokers report feeling unable to go more than a few hours without smoking. They organize activities around opportunities to smoke and feel anxious in situations where smoking is prohibited. This dependency restricts freedom and creates constant preoccupation with tobacco use.
Financial Burden and Stress
The financial impact of smoking tobacco adds substantial stress. With cigarette prices exceeding $8 per pack in many states, a pack-a-day smoker spends over $2,900 annually on cigarettes alone. This expense strains household budgets, particularly for lower-income families where smoking rates are disproportionately high.
Beyond direct cigarette costs, smoking increases healthcare expenses dramatically. Smokers pay substantially higher health insurance premiums. They face more frequent medical visits, prescription costs, and potential lost wages due to smoking-related illnesses. The cumulative financial burden over years of smoking tobacco can exceed hundreds of thousands of dollars.
This economic stress creates a painful irony. Many people smoke to cope with stress, yet tobacco use itself becomes a major source of financial and health-related anxiety. The pressure to maintain the habit despite mounting costs traps individuals in continued tobacco use.
Calculate Your Savings: Quitting just one pack per day saves approximately $3,000 per year. Over ten years, that amounts to $30,000 available for other life goals.
Social and Relationship Impacts
Tobacco use increasingly carries social stigma in the United States. Smoking restrictions in public places, workplaces, restaurants, and even outdoor areas limit where people can smoke. Smokers often feel isolated or judged, standing outside in all weather conditions to satisfy their addiction.
Relationships suffer as well. Non-smoking family members, especially children, face health risks from secondhand smoke exposure. Partners may resent the smell, expense, and health concerns associated with smoking tobacco. These tensions create additional stress within households and can strain important relationships.
Health Anxiety and Failed Quit Attempts
As health consequences emerge, many smokers experience significant anxiety about their tobacco use. They understand the risks but feel unable to quit despite multiple attempts. Each failed quit attempt reinforces feelings of helplessness and low self-efficacy.
Research shows that most smokers want to quit. Approximately 70% of adult smokers report wanting to stop completely. However, nicotine addiction makes cessation extremely challenging without support. The cycle of attempting to quit, experiencing withdrawal, and relapsing creates frustration and shame that compound the stress of continued tobacco use.
How We Can Prevent Tobacco Use

Preventing tobacco use requires comprehensive approaches that address multiple factors influencing initiation and sustained use. Effective prevention strategies combine policy changes, education, community programs, and environmental modifications.
Youth Prevention Programs
Preventing youth tobacco use represents the most effective long-term strategy for reducing overall smoking rates among adults. Since most smokers begin during adolescence, interventions targeting young people yield significant public health benefits.
School-based prevention programs teach students about tobacco health effects, media literacy to resist advertising, and skills to refuse peer pressure. These programs work best when they extend beyond single classroom presentations to create comprehensive tobacco-free environments throughout schools and communities.
- Comprehensive smoke-free policies in all public spaces
- Increased tobacco product taxation
- Strong enforcement of youth tobacco sales laws
- Evidence-based school prevention curricula
- Mass media campaigns highlighting health consequences
- Restriction of tobacco advertising and promotion
- Plain packaging requirements for tobacco products
Effective Prevention Approaches
- Scare tactics without support resources
- Single educational sessions without follow-up
- Allowing continued tobacco advertising targeting youth
- Inadequate enforcement of existing laws
- Programs led by tobacco industry (conflict of interest)
- Focus solely on individual choice without policy support
- Ignoring social and environmental factors
Ineffective or Harmful Approaches
Policy and Environmental Strategies
Comprehensive tobacco control policies create environments that discourage tobacco use and support cessation. Smoke-free laws protect non-smokers from secondhand smoke exposure while also reducing cigarette consumption among smokers and encouraging quit attempts.
Tobacco taxation represents one of the most effective prevention tools. Higher cigarette prices significantly reduce smoking rates, particularly among young people and low-income populations who are more price-sensitive. Each 10% increase in cigarette price reduces consumption by approximately 4% among adults and 7% among youth.
Community-Based Prevention
Community-level interventions create supportive environments for tobacco-free living. These programs mobilize local organizations, healthcare providers, schools, businesses, and government agencies to implement coordinated prevention efforts.
- Community coalitions addressing local tobacco use patterns
- Healthcare provider training on tobacco screening and intervention
- Workplace wellness programs promoting tobacco-free workplaces
- Faith-based organization engagement in prevention messaging
- Culturally tailored programs for high-risk populations
The Disease Control Prevention Centers recommend that states invest tobacco tax revenue in comprehensive tobacco control programs. States with well-funded programs show significantly greater declines in smoking rates compared to states with minimal tobacco control investment.
Addressing Emerging Tobacco Products
Prevention efforts must adapt to address new tobacco products, including e-cigarettes and heated tobacco devices. These products appeal to youth through flavors, sleek designs, and marketing that minimizes health risks. Comprehensive regulation of all tobacco products, not just traditional cigarettes, is essential for effective prevention.
Explore Proven Cessation Treatments
Evidence-based cessation treatments significantly increase your chances of quitting successfully. Learn about medications, counseling, and combination approaches that work.
Are Cessation Treatments Really Helpful? Research Evidence

Scientific research overwhelmingly demonstrates that cessation treatments significantly improve quit success rates. While quitting smoking remains challenging, people who use evidence-based treatments are two to three times more likely to quit successfully compared to those who attempt to quit without assistance.
Medication-Assisted Treatment
The U.S. Food and Drug Administration has approved seven cessation medications that effectively reduce withdrawal symptoms and cravings. These medications work through different mechanisms to ease the quitting process.
Nicotine replacement therapy (NRT) includes gum, patches, lozenges, nasal spray, and inhalers. These products provide controlled nicotine doses without the harmful chemicals in cigarette smoke. NRT helps manage withdrawal symptoms while people work on breaking behavioral habits associated with smoking.
| Cessation Medication | Type | Success Rate Increase | Common Uses |
| Nicotine Patch | NRT | Doubles quit rates | Steady nicotine delivery throughout day |
| Nicotine Gum | NRT | 60-70% increase | On-demand craving management |
| Nicotine Lozenge | NRT | 60-70% increase | Discreet craving relief |
| Varenicline (Chantix) | Prescription | Triples quit rates | Reduces nicotine effects and cravings |
| Bupropion (Zyban) | Prescription | Doubles quit rates | Reduces withdrawal and cravings |
| Combination NRT | Multiple NRT | Best outcomes | Patch plus short-acting NRT |
Prescription medications varenicline and bupropion work on brain chemistry to reduce cravings and withdrawal symptoms. Varenicline partially stimulates nicotine receptors while blocking nicotine from cigarettes, making smoking less rewarding. Bupropion, originally developed as an antidepressant, reduces withdrawal symptoms through different neurological pathways.
Behavioral Counseling and Support
Counseling addresses the psychological and behavioral aspects of tobacco addiction. Individual counseling, group sessions, and telephone quitlines all show effectiveness in supporting cessation efforts. Counseling helps identify triggers, develop coping strategies, and maintain motivation throughout the quitting process.
Telephone quitlines offer accessible support regardless of location or schedule. Trained counselors provide personalized advice, help create quit plans, and offer follow-up support. Research demonstrates that quitline counseling increases quit rates by 30 to 50 percent.
Combination Approaches Yield Best Results
The most effective cessation strategy combines medication with behavioral counseling. This dual approach addresses both the physical addiction to nicotine and the psychological habits surrounding tobacco use. Studies consistently show combination treatment produces higher long-term abstinence rates than either approach alone.
“Combining counseling with FDA-approved cessation medications gives smokers the best chance of quitting successfully. We encourage all patients who smoke to use both approaches together.”
Digital and Mobile Interventions
Technology-based cessation tools have emerged as effective supplements to traditional treatments. Smartphone applications provide daily support, track progress, offer coping strategies, and connect users with support communities. Text messaging programs deliver timely encouragement and tips aligned with individual quit dates.
While digital tools show promise, research suggests they work best when combined with other evidence-based treatments rather than as standalone interventions. The convenience and constant availability of mobile support can enhance overall treatment effectiveness.
What Doctors and Medical Professionals Are Saying

Healthcare providers across medical specialties consistently emphasize that tobacco cessation represents the single most important action smokers can take to improve their health. Medical organizations have issued clear guidance on tobacco use and cessation support.
Surgeon General Reports
The U.S. Surgeon General has released comprehensive reports documenting tobacco health effects since 1964. These landmark reports synthesize thousands of scientific studies to provide authoritative conclusions about smoking and health. The Surgeon General reports have established that smoking causes disease and death, nicotine is highly addictive, and quitting has immediate and long-term health benefits.
Recent Surgeon General reports emphasize that no level of tobacco smoke exposure is safe. Even occasional or light smoking poses significant health risks. The reports also highlight emerging concerns about e-cigarette use among youth and young adults, calling for comprehensive regulation of all tobacco products.
Professional Medical Organization Positions
Major medical organizations including the American Medical Association, American Heart Association, American Lung Association, and American Cancer Society maintain strong positions on tobacco control. These organizations advocate for comprehensive tobacco control policies, increased cessation treatment access, and healthcare system changes to prioritize tobacco treatment.
- Every healthcare visit should include tobacco use screening and brief intervention
- Insurance coverage must include all FDA-approved cessation medications without barriers
- Healthcare providers need training on effective cessation counseling techniques
- Electronic health records should prompt providers to address tobacco use
- Healthcare systems should adopt tobacco-free campus policies
Cardiologists note that quitting smoking is more effective at preventing heart attacks than many medications. Oncologists emphasize that tobacco cessation reduces cancer risk substantially, even after years of smoking tobacco. Pulmonologists highlight that lung function improves within months of quitting, slowing the progression of respiratory disease.
Clinical Practice Guidelines
The U.S. Public Health Service Clinical Practice Guideline provides evidence-based recommendations for treating tobacco use and dependence. These guidelines direct all healthcare providers to consistently identify tobacco users, advise them to quit, assess readiness to quit, assist with evidence-based treatment, and arrange follow-up care.
Doctors emphasize that addiction is a chronic medical condition requiring ongoing management, not a moral failing or simple lifestyle choice. This perspective reduces stigma and encourages people who smoke to seek medical help for cessation just as they would for any other chronic disease.
Ask Your Doctor: Healthcare providers can prescribe cessation medications, provide counseling resources, and create personalized quit plans tailored to your specific needs and health conditions.
Benefits Timeline According to Medical Research
Medical research has documented a clear timeline of health improvements following smoking cessation. These benefits begin almost immediately and continue accumulating over years.
Healthcare professionals consistently communicate that quitting at any age provides substantial health benefits. The body begins healing from tobacco damage remarkably quickly once smoking stops.
Tobacco Use Statistics Over 100 Years in the USA
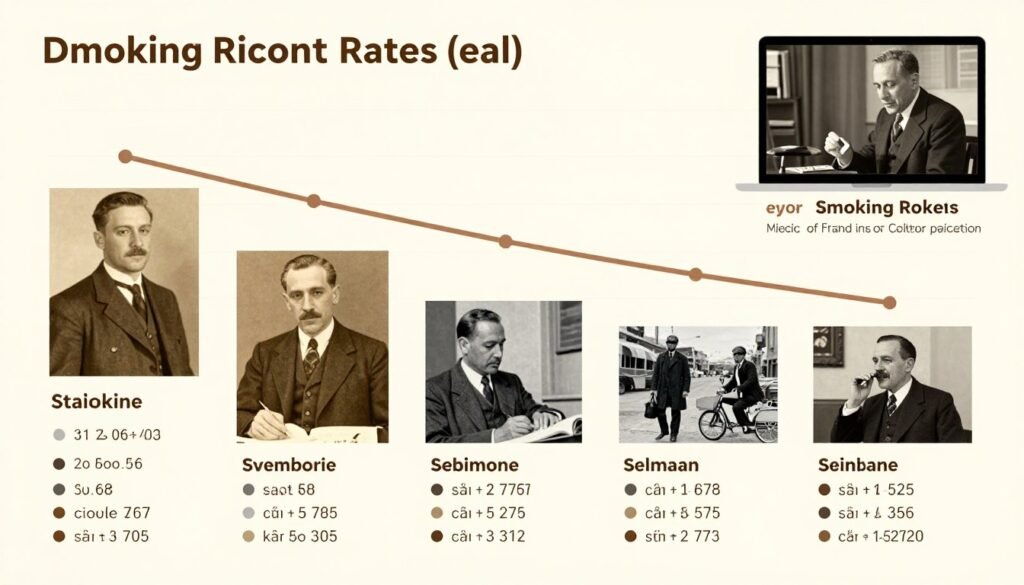
Examining tobacco use patterns over the past century reveals dramatic shifts in smoking prevalence, public awareness, and health policy. This historical perspective demonstrates both the magnitude of the tobacco epidemic and the effectiveness of comprehensive tobacco control efforts.
| Decade | Adult Smoking Rate | Annual Cigarette Consumption (billions) | Major Events/Policies | Public Health Understanding |
| 1900s | ~4% (primarily men) | 2.5 | Cigarettes gaining popularity over cigars and pipes | Limited awareness of health risks |
| 1910s | ~8% | 17 | WWI increases cigarette use among soldiers | Tobacco considered harmless or beneficial |
| 1920s | ~15% | 80 | Women’s smoking becomes socially acceptable | Some concerns emerge but widely dismissed |
| 1930s | ~25% | 130 | Great Depression, tobacco farming subsidized | Early research linking smoking to cancer begins |
| 1940s | ~40% | 280 | WWII, free cigarettes to troops | Scientific evidence accumulating |
| 1950s | ~45% (peak) | 380 | Multiple major studies link smoking to cancer | Medical consensus emerging on health dangers |
| 1960s | ~42% | 510 | 1964 Surgeon General Report, warning labels required | Definitive proof of health harm established |
| 1970s | ~37% | 615 | Broadcast advertising ban, nonsmokers’ rights movement | Secondhand smoke dangers recognized |
| 1980s | ~30% | 630 | Workplace smoking restrictions expand | Nicotine addiction mechanisms understood |
| 1990s | ~25% | 480 | State tobacco lawsuits, Master Settlement Agreement | Comprehensive control strategies developed |
| 2000s | ~21% | 380 | Smoke-free laws proliferate, tobacco tax increases | Evidence-based cessation treatments expand |
| 2010s | ~15% | 250 | FDA tobacco regulation, e-cigarettes emerge | New tobacco product regulation needed |
| 2020s | ~12% | 200 | Continued decline, flavored tobacco restrictions | Focus on health equity and emerging products |
This data illustrates the dramatic rise and subsequent decline of cigarette smoking among adults in the United States. The peak smoking rate of approximately 45% in the 1950s and early 1960s represented a massive public health crisis affecting nearly half the adult population.
The steady decline since the 1964 Surgeon General Report demonstrates the effectiveness of comprehensive tobacco control efforts. Over five decades of sustained public health action reduced adult smoking rates by more than 70 percent from peak levels.
Despite this progress, tobacco use still causes more disease and death than any other preventable cause in the United States. Approximately 34 million American adults currently smoke cigarettes. Continued efforts remain essential to further reduce tobacco use and protect public health.
Can People Quit Permanently or Is Tobacco a Chronic Addiction?

Tobacco addiction has characteristics of a chronic condition, yet millions of people have quit smoking permanently. Understanding this apparent paradox helps set realistic expectations while maintaining hope for successful cessation.
Chronic Disease Model of Addiction
Medical science recognizes tobacco addiction as a chronic, relapsing condition similar to other chronic diseases like diabetes or hypertension. This perspective acknowledges that addiction involves lasting changes to brain structure and function that persist even after someone stops using tobacco.
Like other chronic conditions, tobacco addiction often requires ongoing management rather than a single treatment episode. Many people make multiple quit attempts before achieving long-term abstinence. These attempts are not failures but rather steps in the recovery process, providing learning experiences that inform future efforts.
However, the chronic disease model does not mean quitting is impossible. Rather, it emphasizes that sustained recovery may require continued attention, support, and sometimes treatment adjustments over time. This perspective reduces shame around relapse and encourages persistent effort toward cessation.
Evidence for Permanent Cessation
Millions of Americans have successfully quit smoking tobacco and remained abstinent for years or decades. Currently, there are more former smokers than current smokers in the United States, demonstrating that permanent cessation is achievable.
Success Statistics
- Over 55 million Americans are former smokers
- Approximately 7% of smokers successfully quit each year
- After five years tobacco-free, relapse rates drop significantly
- Long-term abstinence becomes more stable over time
Research shows that cravings and withdrawal symptoms diminish substantially within the first few months of quitting. While occasional cravings may persist, their intensity and frequency decrease dramatically over time. Most former smokers report that quitting becomes easier as time passes.
Long-term follow-up studies demonstrate that people who remain smoke-free for one year have an excellent chance of permanent abstinence. After five years without tobacco, the risk of returning to regular smoking becomes very low.
Factors Supporting Permanent Cessation
Several factors increase the likelihood of achieving permanent cessation. Using evidence-based cessation treatments significantly improves outcomes. Developing strong coping strategies for managing triggers and stress without tobacco proves essential. Building a supportive environment that reinforces the decision to quit helps maintain motivation over time.
Personal health improvements following cessation provide powerful reinforcement. As people experience better breathing, increased energy, improved taste and smell, and reduced coughing, these tangible benefits strengthen commitment to remaining tobacco-free.
Managing the Risk of Relapse
Even after long periods of abstinence, certain situations can trigger powerful cravings. High-risk situations include periods of high stress, alcohol consumption, being around other smokers, and major life changes. Awareness of these triggers allows former smokers to develop strategies for managing them without returning to tobacco use.
If relapse occurs, it does not erase previous progress or mean permanent abstinence is impossible. Most successful quitters made multiple attempts before achieving lasting cessation. Each quit attempt provides valuable information about effective strategies and challenging situations that require additional support.
“The majority of successful ex-smokers required multiple quit attempts. Perseverance and learning from each attempt ultimately leads to permanent cessation for millions of Americans.”
Healthcare providers emphasize viewing cessation as a process rather than a single event. This perspective normalizes the challenges of quitting while maintaining optimism about eventual success. With appropriate support and evidence-based treatment, permanent cessation is an achievable goal for most people who smoke.
What Lifestyle Factors Lead to Tobacco Use and Addiction?

Tobacco use and addiction result from complex interactions among biological, psychological, social, and environmental factors. Understanding these influences helps identify intervention points and target prevention efforts effectively.
Socioeconomic and Educational Factors
Smoking rates vary significantly across socioeconomic groups. Adults with lower educational attainment and income levels smoke at substantially higher rates than those with college degrees and higher incomes. Approximately 21% of adults without a high school diploma smoke, compared to only 7% of those with undergraduate degrees.
Multiple factors contribute to these disparities. Lower-income communities often face higher tobacco product availability, more tobacco advertising, greater exposure to others who smoke, and increased life stressors. Limited access to healthcare and cessation services creates additional barriers to quitting.
Economic stress can both initiate and perpetuate smoking tobacco. People facing financial hardship may turn to cigarettes as an affordable coping mechanism, despite the long-term costs. The immediate stress relief provided by nicotine creates a reinforcing cycle that becomes increasingly difficult to break.
Social and Environmental Influences
Social networks powerfully influence tobacco use patterns. People whose friends, family members, or partners smoke are significantly more likely to smoke themselves. This social clustering of tobacco use reflects both direct social influence and shared environmental exposures.
Family Influence
Children of parents who smoke are three times more likely to become smokers. Early exposure normalizes tobacco use and creates familiarity with smoking behaviors that increase later uptake risk.
Peer Pressure
Adolescents and young adults face significant peer influence regarding tobacco experimentation. Social acceptance within peer groups often motivates initial tobacco use during formative years.
Workplace Culture
Work environments where smoking is common and breaks involve tobacco use create contexts that encourage continued smoking among adults and may promote initiation among non-smokers.
Mental Health and Stress
Mental health conditions are strongly associated with tobacco use. People with depression, anxiety, schizophrenia, or other psychiatric conditions smoke at rates two to three times higher than the general population. Approximately 40% of cigarettes in the United States are smoked by people with mental health or substance use disorders.
Many individuals use tobacco as a form of self-medication to manage mood symptoms, anxiety, or stress. While nicotine provides temporary relief, tobacco use ultimately worsens mental health outcomes and complicates treatment for psychiatric conditions.
Chronic stress from work demands, financial pressures, relationship problems, or caregiving responsibilities contributes to both tobacco initiation and maintenance of addiction. Smoking becomes an ingrained coping mechanism for managing overwhelming stressors.
Marketing and Accessibility
Tobacco industry marketing has historically targeted specific populations through carefully designed advertising campaigns. Despite advertising restrictions, tobacco companies continue promoting products through price discounts, point-of-sale displays, and emerging digital marketing channels.
The widespread availability of tobacco products makes them easily accessible. Tobacco is sold in approximately 375,000 retail locations across the United States. This ubiquitous presence creates constant environmental cues that can trigger cravings and impulse purchases.
Early Life Experiences
Adverse childhood experiences, including abuse, neglect, household dysfunction, and trauma exposure, significantly increase later tobacco use risk. Children experiencing multiple adverse events are more likely to begin smoking during adolescence and develop nicotine dependence.
These early life stressors may alter stress response systems and increase vulnerability to addiction. Tobacco use often represents an attempt to cope with unresolved trauma and emotional distress originating in childhood.
What Kind of Habits Can Change or Overcome Tobacco Addiction?

Successfully overcoming tobacco addiction requires developing new habits and coping strategies to replace smoking behaviors. These habit changes address both the physical addiction to nicotine and the psychological routines surrounding tobacco use.
Physical Activity and Exercise
Regular physical activity provides multiple benefits for people quitting smoking. Exercise reduces withdrawal symptoms, decreases cravings, manages stress, prevents weight gain, and improves mood through natural endorphin release.
Even moderate exercise like brisk walking for 30 minutes can significantly reduce cigarette cravings. Physical activity also serves as a healthy replacement behavior during times when someone would typically smoke. Establishing an exercise routine creates structure and provides achievement milestones that reinforce commitment to quitting.
Recommended Physical Activities
- Brisk walking or jogging when cravings occur
- Yoga or stretching for stress management
- Swimming or cycling for cardiovascular health
- Strength training to build confidence and routine
- Group fitness classes for social support
- Outdoor activities to change environment
Stress Management Techniques
- Deep breathing exercises throughout the day
- Meditation or mindfulness practice
- Progressive muscle relaxation
- Journaling to process emotions
- Adequate sleep for emotional regulation
- Time management to reduce overwhelm
Behavioral Substitutions
Identifying triggers and developing alternative responses proves essential for breaking smoking habits. Behavioral substitutions provide immediate actions to take when cravings occur, helping bridge the time until the urge passes.
Effective substitutions match the sensory and behavioral aspects of smoking. For hand-to-mouth habits, options include drinking water through a straw, chewing gum, eating crunchy vegetables, or using a stress ball. For oral stimulation, sugar-free gum or hard candies provide temporary distraction from cravings.
Environmental Modifications
Changing the environment removes smoking-related cues and makes tobacco use less automatic. These modifications include removing all cigarettes, lighters, and ashtrays from living spaces, cars, and workplaces. Deep cleaning removes smoke odors that can trigger cravings.
Avoiding specific locations and situations associated with smoking during early cessation helps prevent relapse. This might mean taking different routes to work, avoiding certain social situations temporarily, or changing daily routines to break established smoking patterns.
Helpful Habit Changes
- Establishing morning routines without cigarettes
- Drinking water frequently throughout the day
- Taking different breaks at work
- Practicing delay tactics when cravings occur
- Seeking social support from non-smoking friends
- Celebrating milestones and tracking progress
- Using positive self-talk and affirmations
Habits to Avoid
- Excessive caffeine or alcohol consumption
- Spending time with people who smoke
- Skipping meals leading to blood sugar drops
- Neglecting stress management practices
- Isolating from supportive relationships
- Keeping “emergency” cigarettes available
- Testing willpower by exposing oneself unnecessarily
Social Support and Accountability
Building supportive relationships enhances cessation success. Telling family, friends, and coworkers about quit plans creates accountability and opportunities for encouragement. Joining support groups connects people with others facing similar challenges, providing mutual understanding and practical advice.
Online communities and smartphone apps offer 24/7 support and tracking tools. These platforms allow users to share experiences, celebrate milestones, and receive encouragement during difficult moments. The sense of community reduces isolation and normalizes the challenges of quitting.
Mindfulness and Cognitive Strategies
Mindfulness practices help people observe cravings without automatically acting on them. By recognizing that cravings are temporary sensations that will pass, individuals can ride out urges without smoking. This awareness breaks the automatic link between craving and cigarette use.
Cognitive strategies involve challenging thoughts that promote smoking. Instead of “I need a cigarette,” reframing to “I want a cigarette but I don’t need one” or “This craving will pass in a few minutes” empowers people to make conscious choices rather than responding reflexively.
Healthy Nutrition Habits
Maintaining stable blood sugar through regular, balanced meals helps manage mood and reduces cravings. Some people experience increased appetite after quitting smoking. Planning healthy snacks and staying hydrated prevents using food as an unhealthy cigarette substitute while supporting overall wellness.
Certain foods may make cigarettes taste worse, including fruits, vegetables, and dairy products. Incorporating these into diet can serve as natural deterrents while providing nutritional benefits that support recovery.
Moving Forward: Taking Action Against Tobacco Use Health Threat USA

Tobacco use health threat USA remains a critical public health challenge requiring sustained attention and comprehensive action. While significant progress has been achieved over the past decades, millions of Americans continue to suffer from tobacco-related diseases each year.
The evidence is clear: tobacco use causes devastating health consequences, nicotine addiction is powerful but treatable, and evidence-based cessation treatments work. Understanding tobacco as both a preventable health threat and a chronic addiction helps frame appropriate individual and societal responses.
For individuals who smoke, quitting represents the most important action possible to improve health and extend life. Support is available through healthcare providers, telephone quitlines, online resources, and community programs. Combining cessation medications with behavioral counseling offers the best chance of success.
At the community level, comprehensive tobacco control policies create environments that discourage tobacco use and support cessation. Continued advocacy for smoke-free laws, tobacco taxation, youth prevention programs, and equitable access to treatment services remains essential.
The journey from tobacco use to a smoke-free life challenges individuals, but millions have successfully made this transition. With proper support, evidence-based treatment, and persistence through setbacks, permanent cessation is achievable. The health benefits begin immediately and continue accumulating over years and decades.
Start Your Quit Journey Today
You don’t have to quit alone. Free, evidence-based support is available right now through the National Quitline. Trained counselors can help you create a personalized quit plan, access cessation medications, and provide ongoing encouragement throughout your quit journey.
Services are available 24/7 in multiple languages. All resources are free and confidential. Take the first step toward a tobacco-free life today.
Progress against tobacco use health threat USA depends on continued commitment from individuals, healthcare systems, communities, and policymakers. Together, these efforts can create a future where tobacco-related disease and death become truly rare occurrences rather than leading causes of preventable mortality.